In order for the work of the enterprise to always have a positive trend, it is necessary ...


Speaking in an accessible language, not oversaturated with incomprehensible medical terminology, then hypoxia is oxygen starvation, sometimes leading to serious consequences.
Hypoxia is oxygen starvation
There are several types of this fairly common disease:
Next, we will learn more about hypoxia and get acquainted in more detail with those of its types that are most common, and also find out what causes lead to the appearance of this far from harmless disease. In addition, we will determine what symptoms can be considered an alarm signal, and most importantly, how to treat hypoxia in young children and adults.

Hypoxia in pregnant women is a very common occurrence.
If you are planning a pregnancy or, moreover, are in an interesting position, then you should learn as much as possible about the pitfalls that may appear on the way to happy motherhood. After all, it’s not for nothing that they say: “Forewarned is forearmed.”
We sincerely hope that such an unpleasant phenomenon as fetal hypoxia will not affect you. Well, if such an unforeseen situation has already happened and this diagnosis has sounded from the lips of the doctor - do not despair. To get started, read this article to learn more about what lies behind the words symptoms of fetal hypoxia and what are its consequences for the child.
Hypoxia during pregnancy is a fairly common phenomenon, and every year the number of women who experience this disease is only increasing. Fetal hypoxia refers to the processes due to which pathologies begin to appear in the body of a child in the womb. Such processes occur due to insufficient oxygen supply to the organs of the fetus. But because of such changes, not only the child suffers, but also the mother, since they are a single whole, and everything that is bad for the mother is harmful for the baby. Therefore, it is worth making a small clarification: hypoxia is the result of various disorders in the mother's body, which, accordingly, leads to various disorders in the child's body.
Hypoxia during pregnancy is a very alarming bell, especially if it was observed throughout all or almost all trimesters of pregnancy. In such cases, hypoxia is called chronic fetal hypoxia. As a result of chronic hypoxia, irreversible pathological processes in the organs may begin in the fetus. Therefore, do not treat this problem lightly, do not ignore this disease, relying on the fact that everything will pass by itself. It can pass on its own, but time will be lost, and it is not known what problems will arise in the future.

The consequences of hypoxia can affect the further development of the child
The causes of hypoxia are:
The consequences of hypoxia for the fetus are very deplorable - a lack of oxygen leads to the fact that all organs of the fetus are laid incorrectly, due to which their underdevelopment is observed. A child with a high degree of probability, even in the prenatal period, develops malformations that can lead to spontaneous miscarriage. As you can see, intrauterine fetal hypoxia is far from harmless.
If we talk about the consequences of hypoxia in newborns, then the situation is not encouraging either: a child can be born, firstly, much earlier than the due date, which means that the child will be premature. Secondly, a baby can be born already initially with problems in the development of organs. In the worst case, organ damage caused by hypoxia may be incompatible with life.

A healthy lifestyle and frequent walks during pregnancy are the best prevention of hypoxia
In order for a child to be born healthy and avoid hypoxia, one should first of all lead a healthy lifestyle. What is meant by this? The first step is to stop smoking and drinking alcohol. Secondly, you need to eat well and breathe fresh air as often as possible. If the expectant mother has the opportunity to live outside the city for some time, this is very good.
Fresh air, nature, birds singing, silence - all this has a great effect on both the mother's body and the baby's body, saturating his organs with the necessary amount of oxygen. As you can see, the prevention of fetal hypoxia is quite simple. All it takes is positive emotions, a proper lifestyle and regular walks in nature. The importance of the absence of stress should be understood by the relatives of the expectant mother, so as not to worry her over trifles.
As for the treatment of fetal hypoxia, everything is much more complicated here, because in this case the disease is easier to prevent than to treat. The first thing to do is to diagnose and establish the causes that led to this disease. In mild cases, it is enough to simply correct the lifestyle of a pregnant woman, prescribe special vitamin preparations.
If hypoxia has raged in earnest, then here it is necessary to fulfill all the doctor's prescriptions, take the pills prescribed by the doctor, and most importantly - do not be nervous! The emotional background of a pregnant woman greatly affects the child, and can further aggravate the disease.
First of all, the brain suffers from hypoxia, because it is very sensitive to oxygen starvation, especially if it lasts long enough. Hypoxia of the brain can appear in both children and adults. Why is this happening? If we talk about children, then, as mentioned above, their hypoxia manifests itself even in the prenatal period.
It is quite common that a child can earn hypoxia during childbirth if he for a long time is without normal access to oxygen. As a consequence of this disease, children tend to develop such ailments as encephalopathy, epilepsy and other diseases.
If we talk about adults, then it’s clear here too - there’s no way without oxygen. Or rather, without enough oxygen. Why does brain hypoxia occur in adults?
Let's try to name the main reasons (there are two types of reasons - endogenous and exogenous):
- stay in a room that has not been ventilated for a long period;
- inhalation of toxic substances. Often this does not happen on purpose, for example, by workers at various chemical plants, because even if safety standards are observed, harmful vapors are often still emitted, albeit in small quantities. It is the lack of good ventilation plus harmful fumes that eventually lead to the appearance of symptoms of hypoxia;
- very often there is hypoxia in climbers when they conquer the next peak. This is explained by the fact that the higher you go up, the less the air is saturated with oxygen, and this causes unpleasant symptoms that are characteristic of hypoxia;
- unhealthy lifestyle: alcohol consumption, smoking, drug addiction become the causes of the development of the disease;
— medications, which are not taken according to the instructions, can also cause hypoxia;
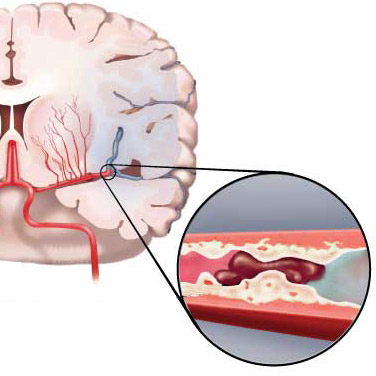
- diseases such as stroke, heart and lung failure also lead to hypoxia;
- anemia;
- spasms of blood vessels that cause circulatory disorders.

Hypoxia often appears in climbers
Symptoms of brain hypoxia. Now a few words about the symptoms that indicate hypoxia in adults:
- excessive drowsiness, when even after waking up a person feels sleepy and overwhelmed;
- fast fatiguability;
- attention is noticeably impaired, it is difficult to concentrate on one thing;
- coordination of movements is fuzzy, a person with hypoxia may experience unsteadiness in movements;
— headache is pulsating in nature, in most cases localized in the frontal part;
- the skin of a person suffering from hypoxia is pale, takes on an unhealthy appearance;
- tachycardia;
- too fast breathing.
Of course, the presence of these symptoms is not yet a guarantee that a person will definitely be diagnosed with hypoxia, but if you observe all or several symptoms in yourself, this is a good reason to consult a doctor and undergo a diagnosis. In most cases, after the examination and finding out the causes of the onset of the disease, the doctor will offer to adjust the lifestyle in order to get rid of hypoxia. But there are times when you need to undergo serious treatment in order to feel good again and protect yourself from irreversible changes in the body.
There is also such a thing as tissue hypoxia. This type of disease can occur in the fetus, and in children, and in adults. Tissue hypoxia is much less common than brain hypoxia, but, nevertheless, many people suffer from this disease. The disease is manifested by oxygen starvation of cells, which can be expressed in membrane damage, vitamin deficiency and a number of other factors. Cyanide poisons, or rather, poisoning with these poisons, lead to tissue hypoxia.
Hemic hypoxia is another type of hypoxia that can significantly reduce the quality of life. This type of hypoxia is also called blood hypoxia, since there is a decrease in the transport of oxygen through the blood. If hemic hypoxia is diagnosed, then anemia will be its obligatory companion, there is a direct relationship between these diseases.
One of the causes of blood hypoxia is carbon monoxide poisoning. In the case of mild poisoning, it is enough to simply transfer the person to fresh air, and over time, the symptoms of hypoxia will disappear. If anemia becomes the culprit for the onset of the disease, then here you will have to use drugs that can increase the number of red blood cells and hemoglobin and thereby relieve the disease.

Warty birch sap will help overcome the disease
ethnoscience has been used since ancient times, because even in ancient times people knew ways to help overcome the disease. Of course, in many cases, medications are indispensable, but folk remedies should not be written off. Plants such as wood lice and warty birch have proven themselves well in the fight against hypoxia. There are many different recipes that tell you how to properly brew these herbs to achieve the desired effect. You just need to opt for the one that seems most convenient to you.
Take a thermos, pour wood lice into it (the grass must be dried) - 1 tbsp. spoon, pour boiling water, then leave for 8-10 hours. The herbal infusion is taken before meals, no more than four times a day. The maximum dose at a time is 50 grams. Warty birch sap should be taken every day for as long as you want. But not more than one liter.
Before starting treatment folk remedies Be sure to check if you are allergic to these herbs. It is also advisable to consult with your doctor, and only if he approves of your choice, proceed to the chosen type of treatment.
As for pregnant women, a lot of herbs are contraindicated for them, since some plants have abortive properties. Given this fact, herbal medicine in pregnant women in many cases is contraindicated or, if allowed, it should be carried out under the constant supervision of the attending physician.
Any kind of hypoxia develops when there is not enough oxygen supplied to the body.
- spend more time outdoors;
- ventilate the premises as often as possible;
- consume more vitamins or take vitamin complexes prescribed by a doctor;
- and for pregnant women, advice is to be less nervous.
It seems that everything is so simple, but why then do so many people suffer from hypoxia? This is because most often few people pay attention to such trifles. Most modern urban residents lead a sedentary lifestyle: home - car - work - car - home, which reduces the time spent outdoors to a minimum. The consequences of hypoxia are very serious, especially for the fetus or for newborns. So take care of yourself, take care of your kids, and let all ailments bypass you!
The respiratory system provides the body with oxygen and removes carbon dioxide. The ratio of these components in the blood must be such that the body functions at the proper level. Different fluctuations up and down in one of the indicators lead to different symptoms. One such condition is hypoxia.
What is hypoxia (anoxia, hypoxemia)? This is a state of the body in which in some areas or in general there is a lack of oxygen in the tissues or a violation of its utilization due to oxidation.
According to the rate of development, hypoxia is divided:
The causes of hypoxia are distinguished by multiple factors:
According to etiology, the following types are divided:
Symptoms of hypoxia depend on the extent of oxygen starvation inside the body. Common features considered to be:
Often, signs of hypoxia are observed in people in large cities who live in a polluted atmosphere, in a constant work mode and are exposed to various chemicals and electronic stimuli.
In the acute form of hypoxia, signs similar to alcohol intoxication are observed:
In chronic hypoxia, which often develops on hills and in a rarefied atmosphere, the following signs are distinguished:
The main diagnosis of hypoxia is a general examination of the patient and analysis of the composition of his blood. First of all, the level of oxygen is determined, and then the reasons for its absence in a normal amount are already sought.
The main methods of treating hypoxia are medicines: antioxidants and antihypoxants. They contribute to the "economical" consumption of oxygen by tissues, better utilization and reduction of hypoxia. Plants with antihypoxic properties are also used. Antihypoxants of a pharmacological nature are often used in acute hypoxia, and of plant origin in chronic hypoxia.
Various instrumental ways introducing oxygen into the body (oxygen therapy with diacarb, oxygen therapy) and increasing blood pressure. Red blood cell transfusion is also used.
As a preventive measure, you should undergo a constant examination by a doctor, and also avoid those places where hypoxia occurs. It is necessary to follow a carbohydrate diet and consume vitamins, treat diseases of the respiratory and other systems in a timely manner.
How long do people live with hypoxia? It all depends on the body of the individual. Modern methods treatments easily remove this syndrome. Life expectancy during hypoxia depends on the state of the body, its internal reserves and "wear and tear". If the body is not able to compensate for the lack of oxygen, then it dies. This can happen both during the day and after a few years.
The prognosis of life is significantly worsened by the fact that oxygen starvation provokes the development of disorders in various body systems. And they, in turn, will lead to the development of other diseases that can be fatal. This makes hypoxia a dangerous syndrome that must be treated on an ongoing basis in cases of recurrent occurrence.
The term "hypoxia" means an abnormal state of the body, which develops when the enrichment of tissues and cells of the body with oxygen stops, as well as under adverse factors in which oxygen is not absorbed by the tissues. Hypoxia of the brain is a whole chain of circumstances and responses of the body that occurs when the incoming volume of oxygen does not correspond to the needs of the brain cells in it, leading to oxygen starvation of the brain. The state of hypoxia occurs in adults, as well as children, and an unborn baby is also capable of experiencing a lack of oxygen.
Fetal hypoxia is a very dangerous condition, the reasons why it develops may be different, but it always leads to serious consequences, which are directly dependent on the time of its occurrence. At the initial stage of pregnancy, this can cause a slowdown in the development and pathology of the fetus; in the later stages, it can cause significant disturbances in the central nervous system. With placental abruption, acute hypoxia develops, from which the baby may die. Intrauterine hypoxia also leads to delays in the development of the fetus, to difficulties in adapting the child to postpartum period and to various neurological disorders: restless sleep, poor appetite, whims, convulsions.
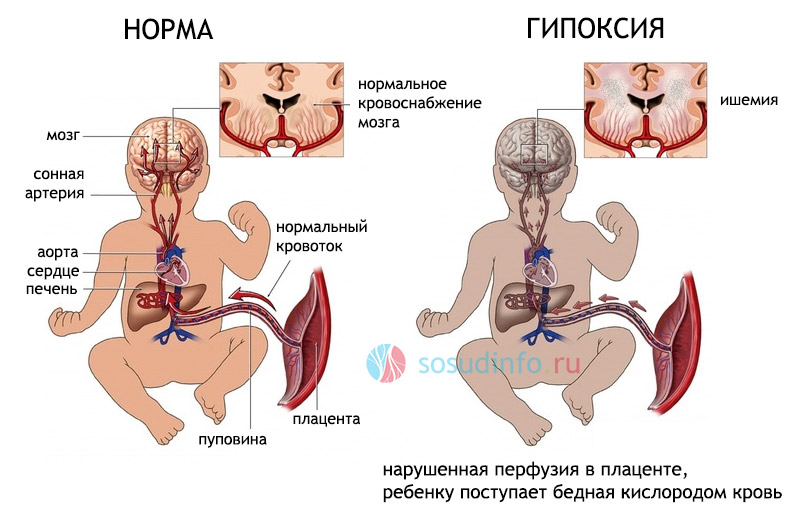
These complications are due to the fact that the body of the unborn child during hypoxia triggers the action of mechanisms aimed at increased blood supply to vital organs - the heart, adrenal glands, brain tissues, and in gastrointestinal tract, kidneys, lungs, and in the skin, the strength of blood flow decreases. Therefore, a child diagnosed with "Intrauterine hypoxia" may be born with possible dysfunctions of these organs. This manifests itself in the form of respiratory disorders, fluid retention in the body, and frequent regurgitation. The next stage, which is characterized by the appearance of signs of oxygen starvation and nervous exhaustion, occurs if oxygen starvation proceeds for a long time. In this condition, the heart rate slows down, the tone of the blood vessels drops, swelling of the tissues of the body occurs, while the brain suffers, nerve cells die, other vital organs are unable to perform their functions, and in the future there is a danger to the life of the child. During the period of gestation, the fetus receives through the placenta all the substances and trace elements necessary to maintain vital activity through it, oxygen enters from the mother's blood into the tissues of the fetus. If a pregnant woman suffers from a lack of nutrients, the fetus will also experience inconvenience.
Fetal hypoxia differs in its characteristics, severity of manifestations, the mechanism of its development and the extent of exposure. There are three main types of hypoxia:
This condition can be provoked by some systemic diseases of a pregnant woman, which include the following reasons:
Of great importance in the development of chronic hypoxia in a child are bad habits of expectant mother . A pregnant woman should never drink alcohol or smoke. All toxins, like useful material, enter the blood of the baby and cause negative consequences.
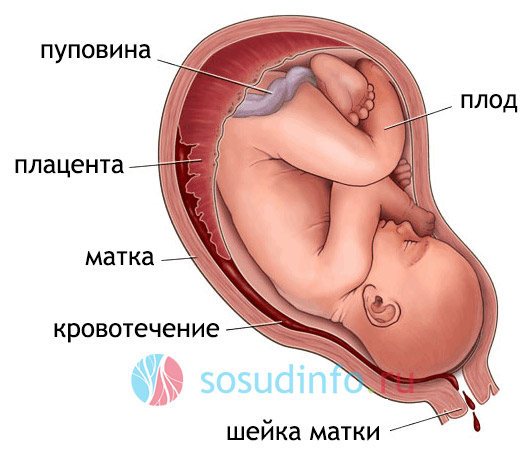
Other good reasons for the development of hypoxia in the child may be possible abnormalities in the development of the placenta, overgestation during pregnancy or increased uterine tone, other deviations from the normal natural algorithm for bearing a child, the most common and dangerous factor for acute intrauterine hypoxia may be premature detachment of a normally located placenta. Fetal hypoxia can also be caused by infection of the fetus in the womb, malformations in its development, incompatibility of the fetal blood with the mother's blood - this condition causes, it is equally dangerous for the unborn child and the woman herself. In severe childbirth, hypoxia of the brain of the newborn may occur, caused by a mechanical factor - prolonged squeezing of the head in the birth canal, entanglement around the neck of the umbilical cord, and also getting into Airways mucus and amniotic fluid. This complication of childbirth is called asphyxia and requires resuscitation. The combination of acute and chronic forms of hypoxia is the most unfavorable in predicting the development of complications in a baby at birth.
The first symptom of fetal hypoxia is the active movements of the child., with this, the baby reflexively tries to increase blood supply, increase blood flow. At first, a woman notes strong and sharp points, violent stirring, it can cause her inconvenience and even pain. If fetal hypoxia increases, its tremors gradually weaken, and may disappear altogether. This sign should alert the woman, let her know that not everything is in order with the baby. In the antenatal clinic, it is recommended that if the pregnancy is more than 28 weeks, keep records of fetal activity.
It is considered normal when a child moves at least 10 times in 12 hours, if there are fewer of them, you need to urgently seek medical help.
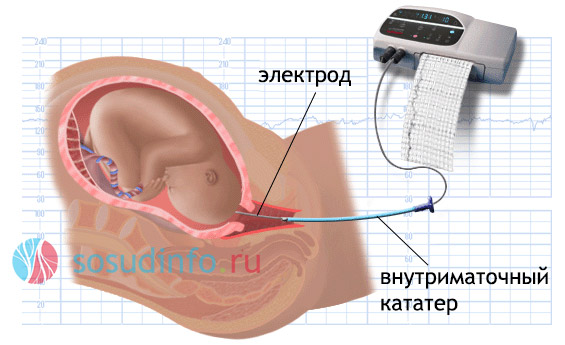
When determining intrauterine fetal hypoxia, obstetricians use complex methods designed to assess the condition of the fetus. These methods include listening to fetal heart sounds using an obstetric device - a stethoscope. The doctor evaluates the heart rate, their tone, rhythm, extraneous noise. But this method cannot be accurate enough, therefore, at the slightest suspicion of hypoxia, cardiotocography should be additionally applied, using a special ultrasonic sensor, in this study, the indicators are recorded on paper and the doctor is able to analyze the fetal heart rate in different parameters. Another method that allows you to explore to determine the deviations in the blood flow between a woman and the fetus is called. Here, blood circulation is assessed in all links of the fetal blood supply chain, the severity of hypoxia and the prognosis for the course of pregnancy depend on the nature of the changes. In addition to the manipulations described, the fetal ECG also provides information about the state of his health, and laboratory tests of the mother's blood for the biochemical composition and levels of pregnancy hormones are also used.
In addition, if there is a suspicion of intrauterine hypoxia, amniotic fluid is analyzed for the presence of meconium, the original feces, in them. Lack of O 2 provokes relaxation of the muscles of the rectum of the baby and meconium enters the amniotic fluid. This method of diagnosis is especially important with increasing labor activity, the whole tactics of the birth process will depend on its results.
If the doctor suggests intrauterine fetal hypoxia, the woman is sent to the hospital for additional examinations and necessary therapy. When the condition of the fetus allows, treatment at home under medical supervision is possible. A prerequisite for the cure of hypoxia is the complete rest of the woman.  Treatment for intrauterine hypoxia should be aimed at ensuring normal blood supply to the fetus, it will depend on the cause of hypoxia and the degree of pathology detected. In most cases expectant mother strict bed rest is prescribed, drugs are prescribed that reduce blood viscosity, improve blood supply to the placenta and normalize the metabolism between the mother and fetus, the predominant position in bed is on the left side. If during the course of the treatment no positive changes are noted, and fetal hypoxia continues to increase, obstetricians may decide to perform a caesarean section when the period exceeds 28 weeks of pregnancy. To prevent such complications, the expectant mother should give up bad habits, spend more time outdoors, not overwork, and lead a healthy lifestyle. Great importance should be given to the prevention of iron deficiency anemia, as one of the main causes of fetal hypoxia. Complete balanced diet, registration for pregnancy in the antenatal clinic in the early stages and timely visits to the doctor will play a huge role in the prevention of fetal hypoxia and its complications. If a pregnant woman was diagnosed with Chronic intrauterine hypoxia, mandatory cardiomotor monitoring of the fetal condition is carried out during childbirth in order to minimize negative consequences for the child.
Treatment for intrauterine hypoxia should be aimed at ensuring normal blood supply to the fetus, it will depend on the cause of hypoxia and the degree of pathology detected. In most cases expectant mother strict bed rest is prescribed, drugs are prescribed that reduce blood viscosity, improve blood supply to the placenta and normalize the metabolism between the mother and fetus, the predominant position in bed is on the left side. If during the course of the treatment no positive changes are noted, and fetal hypoxia continues to increase, obstetricians may decide to perform a caesarean section when the period exceeds 28 weeks of pregnancy. To prevent such complications, the expectant mother should give up bad habits, spend more time outdoors, not overwork, and lead a healthy lifestyle. Great importance should be given to the prevention of iron deficiency anemia, as one of the main causes of fetal hypoxia. Complete balanced diet, registration for pregnancy in the antenatal clinic in the early stages and timely visits to the doctor will play a huge role in the prevention of fetal hypoxia and its complications. If a pregnant woman was diagnosed with Chronic intrauterine hypoxia, mandatory cardiomotor monitoring of the fetal condition is carried out during childbirth in order to minimize negative consequences for the child.
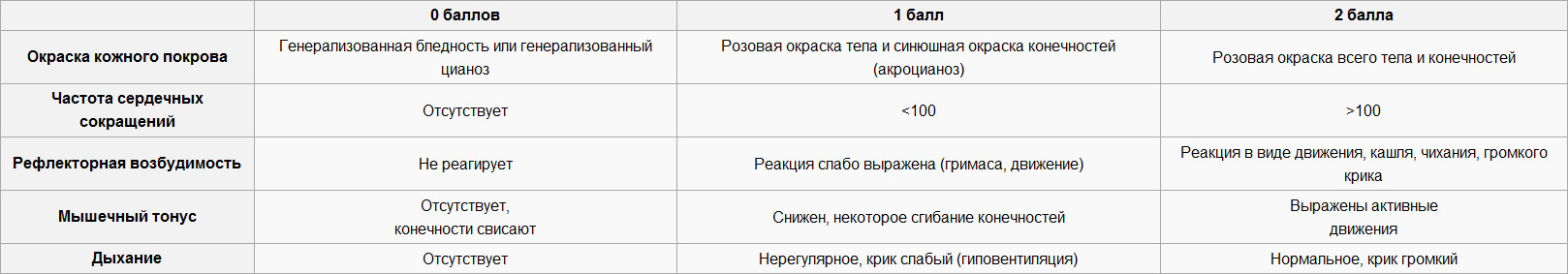
Immediately after birth, when assessing the state of health of the child, the Apgar scale is used, according to which the condition is assessed. skin, reflex excitability and muscle tone. Normally, the indicator should be from eight to ten points, a score below five points means hypoxia, the lower the number of points assigned, the more difficult the child's condition.
(click to enlarge)
With severe hypoxia, the child is pale, muscle tone is reduced, convulsive syndrome, deviations in the functioning of internal organs, up to serious disorders of the central nervous system with the formation of blood clots and are possible. At birth, a child with suspected hypoxia should immediately receive medical care aimed at relieving oxygen starvation: the airways are freed from fluid and mucus, the child is warmed, resuscitation is carried out if necessary, achieving improvement to a state that does not pose a threat to life. After stabilization of the baby's condition, they are placed in a pressure chamber, nutrient solutions are injected, and therapy is carried out aimed at removing the manifestations of hypoxia. In the first month of life, the baby after undergoing hypoxia is restless, easily excitable, his muscle tone is increased, which manifests itself in involuntary twitching of the arms, legs, chin, and are possible. In other cases, lethargy, unwillingness to breastfeed, he is worried about frequent regurgitation. The older the baby becomes, the less noticeable these manifestations are, however, at 5-6 months, the initial symptoms may return: convulsions may occur again, muscle tone may increase. This period can last for several months or several years, it will depend on the degree of damage to the brain of the baby and his ability to recover. The consequences of hypoxia of the brain of the fetus and newborn are very serious, up to the death of the baby Therefore, it is very important to identify this condition in time and take measures to prevent complications in the child's health in the future.
Further a baby who has undergone intrauterine hypoxia should be constantly registered with a neurologist so that the doctor has the opportunity to notice pathologies in time in the physical and mental development and prescribe the necessary therapy, since the state of prolonged oxygen starvation can cause various deviations and lags in the development of the baby. To avoid this, it will be necessary to regularly assess his health and carry out appropriate treatment if necessary. To help a newborn baby cope with the effects of hypoxia, parents should provide a calm atmosphere at home, comfortable temperature regime, protect from overheating and hypothermia. You should not swaddle the child tightly, you need to give him the opportunity to move more. The big plus is breast-feeding, warm baths with soothing herbs, special massages and gymnastics, which the pediatrician should teach mom to use. This should be done daily for 2-3 years.  In difficult cases of the course of the disease, as prescribed by the pediatrician, massage should be carried out by a specialist who has the skills to treat diseases nervous system. It is with the help of massage that you can help restore the nervous system and overcome delays in the development of the child. Reflexology has an intense effect on the central nervous system, it is also used as directed by a doctor if hypoxia has caused significant disturbances in the development of the child. There are various methods of reflexology: acupuncture, laser treatment, etc. If indicated, it is advisable to consult with an osteopath discuss with him the feasibility of osteopathic treatment. Help in overcoming the consequences of intrauterine hypoxia can and physiotherapy, this becomes relevant with a delay in the development of motor skills. It should be carried out by a specialist who owns these skills. If there are delays in speech development, you should contact a speech therapist. All of the above activities should be carried out in a strict system, with a certain sequence and under the obligatory supervision of the attending physician, who is able to track the dynamics of the mental and physical development of the child. Self-medication is absolutely unacceptable! With the right and responsible approach to treatment, in most cases it is possible to overcome the negative residual effects of hypoxia and return the child's condition to normal.
In difficult cases of the course of the disease, as prescribed by the pediatrician, massage should be carried out by a specialist who has the skills to treat diseases nervous system. It is with the help of massage that you can help restore the nervous system and overcome delays in the development of the child. Reflexology has an intense effect on the central nervous system, it is also used as directed by a doctor if hypoxia has caused significant disturbances in the development of the child. There are various methods of reflexology: acupuncture, laser treatment, etc. If indicated, it is advisable to consult with an osteopath discuss with him the feasibility of osteopathic treatment. Help in overcoming the consequences of intrauterine hypoxia can and physiotherapy, this becomes relevant with a delay in the development of motor skills. It should be carried out by a specialist who owns these skills. If there are delays in speech development, you should contact a speech therapist. All of the above activities should be carried out in a strict system, with a certain sequence and under the obligatory supervision of the attending physician, who is able to track the dynamics of the mental and physical development of the child. Self-medication is absolutely unacceptable! With the right and responsible approach to treatment, in most cases it is possible to overcome the negative residual effects of hypoxia and return the child's condition to normal.
With proper treatment during the first year of life, the child's health should return to normal, but in some cases the consequences of hypoxia can appear even after a rather long period of time. Children may have a delay in speech development, inability to concentrate, restlessness, constant headaches. In the most difficult cases, progressive CNS lesions may develop, such as significant hearing impairment, attention, as well as persistent disorders of the central nervous system, such as epilepsy, other cerebrovascular disorders, including (in rare cases) cerebral venous.
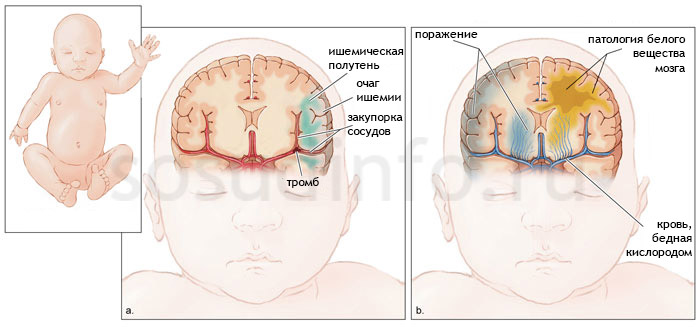
Consequences of hypoxia: stroke (left) and hypoxic-ischemic encephalopathy (right) in a newborn
Not only newborn children can suffer from hypoxia, adults also experience oxygen starvation, the causes of which can be different. As a rule, this condition is caused by chronic diseases.
Hypoxia in adults also leads to disturbances in the functioning of the central nervous system, chronic fatigue syndrome, decreased immunity, sleep disturbances, and general deterioration in health. Various methods are used to treat hypoxia in adults, first of all, it is necessary to treat the underlying disease that caused it.
The use of oxygen cocktails can help to cope with the consequences of hypoxia and improve the quality of life. This invention allows you to restore strength during overwork, saturate cells with oxygen, improve metabolism, increase concentration, attention and reaction, and also has many more positive qualities.  An oxygen cocktail is a thick foam that is completely filled with oxygen molecules. It is prepared on juices, fruit drinks, syrups and enriched with oxygen using special devices, oxygen concentrators. For a long time, oxygen cocktails were available only in medical institutions, but recently compact oxygen cartridges have appeared on sale, this allows you to cook healthy drink Houses. Chronic oxygen starvation of the brain in adults also leads to negative consequences, the destruction of nerve endings and. To prevent this and maintain the quality of life, you should be observed by doctors, monitor your well-being and systematically treat chronic diseases. Postponing the onset of old age and maintaining vigor for many years is quite within the power of everyone who sincerely desires this. To do this, you need very little - to lead a healthy lifestyle, spend more time in the fresh air, relax and value yourself and your health.
An oxygen cocktail is a thick foam that is completely filled with oxygen molecules. It is prepared on juices, fruit drinks, syrups and enriched with oxygen using special devices, oxygen concentrators. For a long time, oxygen cocktails were available only in medical institutions, but recently compact oxygen cartridges have appeared on sale, this allows you to cook healthy drink Houses. Chronic oxygen starvation of the brain in adults also leads to negative consequences, the destruction of nerve endings and. To prevent this and maintain the quality of life, you should be observed by doctors, monitor your well-being and systematically treat chronic diseases. Postponing the onset of old age and maintaining vigor for many years is quite within the power of everyone who sincerely desires this. To do this, you need very little - to lead a healthy lifestyle, spend more time in the fresh air, relax and value yourself and your health.
The term hypoxia refers to the pathological state of the body, due to its oxygen starvation as a whole or individual tissues and organs.
Hypoxia can develop with an insufficient amount of oxygen in the blood, with a lack of it in environment or with biochemical disorders of the tissue respiration process.
The adaptation of the organism to hypoxia in each person is purely individual and therefore oxygen starvation in patients causes various complications, depending on the state of health of individual organs and the whole organism.
Hypoxia can occur in both acute and chronic forms.
The acute form of hypoxia often has a short-term character and usually occurs with high physical activity. This type of hypoxia is observed during fitness classes or long runs. The resulting oxygen starvation quickly passes, because. mobilization of a healthy body includes the mechanisms of adaptation of the body to hypoxia.
An acute form of hypoxia can develop during a stay in a stuffy room. Characteristic signs of hypoxia in this case are drowsiness, lethargy, decreased concentration, yawning. All this takes place when fresh air enters or leaves the room.
But quite often acute hypoxia is caused by pathological processes in the body. This form may be a consequence of heart failure, pulmonary edema, carbon monoxide poisoning, or airway obstruction.
Acute hypoxia can pass very quickly, but can be observed within a few days.
Chronic hypoxia is often observed in diseases of the cardiovascular system and respiratory organs.
The severity of chronic hypoxia depends on the localization of the organ suffering from hypoxia, the duration and type of pathology, the characteristics of the body and metabolic processes in it.
Chronic hypoxia is dangerous because it leads to a decrease in the ability of tissues to absorb oxygen. Thus, a person's chances of recovery are reduced.
This applies to both general and local disease, in which only a certain part of the body is affected. The same applies to atherosclerosis, the development of blood clots, embolism, tumors and edema.
Chronic hypoxia can develop and last from several weeks to several months.
When oxygen starvation occurs in the body, a protective mechanism wakes up, working towards eliminating or reducing the severity of hypoxia.
These processes appear already in the very early stage hypoxia. Such adaptation mechanisms are called emergency. If the disease passes into the chronic stage, then the process of adaptation of organs to hypoxia becomes more complex and lengthy.
Emergency adaptation consists in the transport of oxygen and metabolic substrates and the inclusion of tissue metabolism.
Long-term adaptation is formed more slowly and includes adjustment of the functions of the pulmonary alveoli, pulmonary ventilation blood flow, compensatory increase in the myocardium, bone marrow hyperplasia, and accumulation of hemoglobin.
According to the duration and intensity of the flow, functional, destructive and metabolic hypoxia are distinguished.
Destructive hypoxia is a severe form and leads to irreversible changes in the body.
Functional hypoxia occurs when hemodynamics is disturbed, i.e. due to impaired blood flow various reasons e.g. hypothermia, injuries, burns, etc.
Metabolic hypoxia develops as a result of impaired oxygen supply to tissues. At the same time, there is a change in metabolic processes in them.
Both functional and metabolic hypoxia are reversible. This means that after the necessary treatment or changes in the factors causing hypoxia, all processes in the body are restored.
According to the causes of hypoxia, it is divided into:
Brain hypoxia and neonatal hypoxia are often found in medical practice.
Hypoxia of the brain disrupts the activity of the whole organism and, first of all, the central nervous system.
Hypoxia in newborns is quite common in obstetric and gynecological practice and has serious consequences. The main causes of chronic fetal hypoxia are maternal diseases such as diabetes mellitus, anemia, occupational intoxication, heart disease, and other diseases.
The causes of chronic fetal hypoxia include a complicated pregnancy caused by a disorder of the uteroplacental circulation. In addition, the pathological development of the fetus in the form of malnutrition, Rh conflict, infection of the fetus when protective barriers are broken, and multiple pregnancies can also be causes of chronic fetal hypoxia.
 Signs of hypoxia
Signs of hypoxiaSymptoms of oxygen starvation are expressed by constant fatigue and depression, accompanied by insomnia.
There is a deterioration in hearing and vision, headaches and chest pains appear. Sinus is detected on the electrocardiogram. Patients experience shortness of breath, nausea, and disorientation in space. Breathing may be heavy and deep.
In the initial stage of the development of cerebral hypoxia, its signs are expressed by high energy, passing into euphoria. Self-control over motor activity is lost. Signs may include staggering gait, palpitations, pallor bordering on cyanosis, or vice versa, the skin becoming dark red.
In addition to those common to all, signs of cerebral hypoxia, as the disease progresses, are expressed by fainting, cerebral edema, and lack of skin sensitivity. Often this condition ends in a coma with a fatal outcome.
Any type of hypoxia requires immediate treatment based on the elimination of its cause.
With the onset of pregnancy, colossal changes occur in the mother's body, allowing a new life to arise and develop. A unique mother-placenta-fetus system is formed. Normally, this mechanism works very well, providing the baby with oxygen and nutrients, removing its waste products and protecting it from adverse factors.
Even with a normal pregnancy, the fetus's blood is less oxygenated than the mother's. This deficiency can be compensated for by the increased work of the baby's heart and a special type of hemoglobin - the so-called fetal hemoglobin, which carries oxygen to every cell of the child.
If the blood supply through the placenta is disturbed, then the body of the fetus cannot compensate for everything. Approximately 3-7% of pregnancies occur with a violation of this system. This condition is called fetoplacental insufficiency (FPI), the result of which is intrauterine fetal hypoxia. According to statistics, this condition occurs in 10% of all pregnancies and childbirth.
The placenta completes its formation by the 16th week of pregnancy, by this time the placental circulation begins to fully function, that is, to deliver oxygen-enriched blood through the umbilical vein to the liver and heart of the unborn baby. From there, the blood is distributed to all organs and tissues of the embryo through special connections - shunts. Any disturbance in the blood circulation or in the structure of the placenta leads to the development of FPI.
The placenta and its predecessors undergo two waves of activity during their development: at 7-9 and 14-17 weeks of pregnancy. It is during these periods that vascular anomalies often occur, resulting in FPI. Usually, such disorders are formed against the background of the mother’s illness, an unhealthy lifestyle, or complications of pregnancy.
In view of the formed FPI, intrauterine hypoxia of the baby develops, which means insufficient oxygen supply to his body. Synonyms in intrauterine hypoxia is oxygen deficiency or oxygen starvation of the fetus.
It should be noted that this condition is not a disease. This is a syndrome that develops in an unborn child as a result of various adverse factors affecting his body.
Oxygen starvation of the fetus can develop for a long time and gradually, as a result of chronic renal failure. This hypoxia is also called chronic. If the violation of the blood supply to the placenta developed quickly and rapidly, then FPI and hypoxia are acute.
Also, fetal hypoxia can develop during pregnancy, then it is called antenatal, and if it occurs during childbirth, they talk about intranatal hypoxia.
Almost every expectant mother has a chance of developing hypoxia, but not everyone develops it. The doctor of the antenatal clinic calculates the degree of risk for the occurrence of this condition in the fetus, taking into account the chronic pathology of the mother, endocrine disorders that existed before and appeared during pregnancy and complications of the gestational period:
The causes of intrauterine hypoxia are divided into 2 large groups, depending on whether they contribute to the development of acute or chronic hypoxia.
Chronic oxygen deficiency of the fetus is caused by adverse factors that act for a long time.
During pregnancy, the placenta has a great influence on the woman's heart and blood vessels. The volume of blood almost doubles, and the peripheral vessels dilate, which prevents surges in blood pressure. Therefore, if the tonometer stubbornly shows values more than 130 / 80 mm Hg. column, then you can think about the incorrect work of the mother-placenta-fetus.
The classification of hypertensive disorders during pregnancy is presented in the table.
| Disorder | Definition |
| Chronic hypertension | Hypertension present before pregnancy or first diagnosed before 20 weeks of gestation |
| Preeclampsia-eclampsia |
New onset hypertension during pregnancy (> 140 mm Hg systolic or > 90 mm Hg diastolic pressure) and urinary protein (excretion > 0.3 g per 24 hours) after 20 weeks diabetes and pregnancyDiabetes mellitus is a serious disease that mainly affects the kidneys, blood vessels and nerves. With this pathology, uncontrolled blood sugar levels adversely affect almost all organs and tissues. During pregnancy, diabetes causes fetal hypoxia, putting the health of the baby and mother at great risk. Maternal risk of diabetes:
The risk of diabetes to the fetus:
Planning pregnancy with diabetes
Careful monitoring of fetal health is required throughout pregnancy, including Doppler ultrasound, fetal biophysical profiling, and maternal blood glucose monitoring. The optimal term for delivery is considered to be 38-40 weeks, mainly - independent childbirth. Thyroid diseasesApproximately 5% of pregnant women have an under-functioning thyroid gland. Some of them suffered before pregnancy, and for some it arose during the period of expectation of the baby. This is due to hormonal changes in the body and the increased need for the fetus in trace elements. The main symptoms of hypothyroidism before pregnancy:
Among the consequences of hypothyroidism during pregnancy, fetal growth retardation, fetal hypoxia, placental insufficiency, placental abruption and premature birth are common. In addition, hypothyroidism in a newborn without treatment may develop oligophrenia. The norms of the level of TSH (thyroid-stimulating hormone) for each trimester of pregnancy have not yet been studied, the average data is from 0.4 to 3.5 mU / l. If the amount of the hormone differs from these values, then it is necessary to conduct an ultrasound of the gland and prescribe treatment. Hormone replacement drugs are used to treat hypothyroidism. They are prescribed by a doctor, since it is quite difficult to find the right dose for a woman in position. If hypothyroidism can be compensated with medications, then the risk of complications for the baby is minimized. Infectious diseasesInfections themselves can cause vascular reactions and deterioration of uteroplacental blood flow. For example, with influenza, the risk of fetal hypoxia is quite high, since fever is combined with cough and general intoxication. Some infections (toxoplasmosis, chlamydia, cytomegalovirus, ureaplasmosis and others) are able to cross the placenta, causing inflammation directly in the fetal membranes, placenta and amniotic fluid. In this case, not only FPI and chronic fetal oxygen deficiency develop, but the risk of acute hypoxia and the death of the unborn child also increases. Symptoms that are a reason to visit a doctor:
Most often, after treatment of the infection, the condition of the fetus stabilizes. Among the drugs used are antibiotics, antiviral and antifungal drugs, as well as infusions of intravenous solutions to relieve intoxication. In some cases, it is necessary to use emergency delivery when the life of the mother and child is threatened. Immunological complications during pregnancyRh-conflict during the gestation period occurs in the case of Rh-negative maternal blood and Rh-positive blood in the fetus. The risk group for the development of an immunological conflict (by blood type) includes expectant mothers who have the first blood type (O or I), and the future father has any other, but not the first. Due to immunological incompatibility, immunological complications develop, which are caused by the production of antibodies in the maternal body that adversely affect the tissues and organs of the fetus. Ultimately, the unborn child develops oxygen deficiency. Antiphospholipid SyndromeAntiphospholipid syndrome or APS refers to an autoimmune disease characterized by the production of large amounts of antibodies to phospholipids. Phospholipids, in turn, are necessary for the construction of cell parts. The prevalence of APS is 5% among all expectant mothers. In a third of cases, APS is the cause of habitual miscarriage. If certain measures are not followed during pregnancy and treatment is not carried out, then this syndrome can provoke the occurrence of oxygen starvation and intrauterine growth retardation of the fetus, placental abruption, severe preeclampsia, pulmonary embolism in the mother, and even the death of the baby (in utero) and mother. Factors that provoke the occurrence of APS
PolyhydramniosAn excess amount of amniotic fluid can provoke gestational arterial hypertension, significantly increases the likelihood of entanglement of the fetus (in this case neck) by the umbilical cord and the formation of true knots in the umbilical cord (when the umbilical cord is tied into a knot due to the increased activity of the baby). In addition, polyhydramnios leads to metabolic disorders in the fetus and the gradual development of oxygen deficiency, which in turn delays the growth of the fetus. oligohydramniosThe lack of amniotic fluid reduces the motor activity of the unborn child, and with severe oligohydramnios it can lead to compression of the fetus and the formation of intrauterine anomalies in it. A small amount of water causes disturbances in oxygen metabolism, which causes chronic hypoxia. Also, with oligohydramnios, weakness of the labor force and early postpartum hemorrhage (violation of the contractile activity of the uterus) often develop. OverwearingIf the gestation period exceeds 41 weeks and 3 days, they speak of true overgestation, which can lead to oxygen starvation of the fetus and cause its antenatal death. If there is a suspicion and a threat of overgestation in the absence of labor, doctors carefully recalculate the duration of pregnancy according to various data (the first visit to the antenatal clinic, ultrasound, the last menstruation and the first movement of the fetus). If the diagnosis of true overgestation is confirmed, labor induction and labor induction are resorted to. The tactics of managing a pregnant woman is individual and depends on the maturity of the cervix, the state of health of the woman and the indicators of additional examination of the fetus (ultrasound, CTG, Doppler). Multiple pregnancyMultiple pregnancy is always a high risk of developing chronic hypoxia of one or more fetuses. This is especially true of monochorionic monoamniotic twins, the fetuses of which have common fetal membranes and placenta). As a result, there is a high risk of uneven distribution of maternal blood between future babies, which will lead to insufficient oxygen supply for one of the twins. breech presentationWhen the fetus is presented with the pelvic end, the likelihood of pressing the umbilical cord increases when it passes through the birth canal. In addition, breech presentation provokes various complications in childbirth, which leads to the development of oxygen starvation of the fetus. Fetal malformationsIn the event of intrauterine malformations (anomalies of the cardiovascular system, neural tube, etc.), chronic oxygen deficiency in the fetus occurs in 100% of cases. To exclude malformations, biochemical and ultrasound screening is carried out, the results of which determine the subsequent tactics of managing a pregnant woman and childbirth. Bad habitsIf a pregnant woman has not given up bad habits (smoking, drinking alcohol and psychoactive substances), toxic substances are formed in her body as a result of metabolic disorders, and the vessels are in constant spasm. All this significantly impairs blood supply in the mother-placenta-fetus system and leads to the development of chronic oxygen starvation of the fetus. In addition, regular alcohol intake during pregnancy causes the formation of alcoholic fetopathy of the fetus, which affects its mental and physical development. What causes acute hypoxiaAcute oxygen deficiency of the fetus can develop at any stage of pregnancy, but most often occurs during childbirth. The only true tactic of doctors in acute hypoxia is immediate delivery, since the count goes by minutes and the fetus may die. Placental abruptionPlacental abruption is a formidable complication, the main symptom of which is severe pain in the abdomen, which forces the pregnant woman to take a forced position and, as a rule, bleeding from the birth canal of varying intensity (sometimes there may be no external bleeding, for example, with placental abruption in the bottom of the uterus). This complication threatens not only the life of the fetus, but also the woman. With detachment, there is a “separation” of a section of the placenta from the wall of the uterus, which leads to rupture of blood vessels and disruption of oxygen supply to the fetus. Since detachment occurs ahead of time when the fetus is still in the uterus, the uterine vessels do not have time to shrink and stop blood loss. As a result, severe fetal hypoxia occurs, the consequences of which are difficult to predict. A common cause of detachment is increased arterial pressure, and outpouring of a large volume of water, abdominal trauma. Since 15% of placental abruptions are accompanied by intrauterine fetal death from oxygen starvation, immediate delivery is the best option. Acute violation of the umbilical blood flowThe reasons for this complication are:
The occurrence of these complications can be suspected during ultrasound at 32 to 36 weeks, especially cord entanglement. But by the beginning of labor, the fetus can repeatedly change its location, which will also affect the localization of the umbilical cord. Therefore, in childbirth, it is advisable to carry out cardiotocography. The compression of the umbilical cord is indicated by a decrease in the fetal heart rate during a contraction and a slow recovery of the heart rate after a contraction. In the case of persistent and increasing bradycardia, a caesarean section is indicated. Anomalies of tribal forcesViolation of the contractile activity of the uterus during childbirth (weak contractions, dystocia of the cervix or discoordination of labor forces) delays the process of childbirth, slows down the progress of the fetus along the pelvic ring and tires the woman, which causes acute oxygen starvation in the fetus. Protracted or rapid laborDuring prolonged labor, the fetal head is in the same plane of the small pelvis for a long time, as a result of which the blood vessels are compressed and the blood flow is disturbed. With rapid delivery, the child very quickly passes through all the planes of the small pelvis and does not have time to complete the correct turn by the period of expulsion of the fetus. Premature discharge of waterThe outflow of water before the onset of labor leads to a long anhydrous period, which is dangerous not only for the development of infectious complications, but also for acute oxygen deficiency in the fetus. Rupture of the uterusUterine rupture is an extremely serious and urgent condition, resulting in a sharp cessation of the fetal blood supply, acute hypoxia and antenatal death. The woman's life is also at risk, and if an immediate operation is not carried out, she may die. This complication is predisposed to:
Hypotension in a womanLow blood pressure in the mother, such as fainting, leads to a sharp decrease in blood flow to the fetus and oxygen starvation. To prevent the occurrence of fainting will help rational and good nutrition pregnant women, timely and adequate treatment of anemia during pregnancy and correct breathing and behavior of the woman in labor. During contractions, a woman breathes shallowly and often, which is not true. Such breathing does not saturate the blood with oxygen, tires the woman in labor and causes hypoxia in the fetus. A woman experiences dizziness, shortness of breath, and the baby's heart rate increases. false contractionsFalse or preparatory contractions occur at 22 to 37 weeks and do not lead to structural changes in the cervix. False contractions are characterized by a periodic increase in the tone of the uterus and the occurrence of pulling pains in the lower abdomen. Tension of the uterus (hypertonicity) can cause oxygen starvation of the fetus. Use of drugs in childbirthDuring contractions, narcotic analgesics, such as promedol, are sometimes used. Promedol depresses the respiratory center of the fetus, which provokes the development of oxygen deficiency. The use of drugs in childbirth should be strictly justified and carried out with monitoring (fetal heart rate control, CTG), and the laboring period is carried out in the presence of a neonatologist. Degrees of hypoxia and placental insufficiencyViolation of blood flow in the placenta does not always entail instantaneous hypoxia. The fetus has a certain reserve of “strength” that allows it to compensate for FPI. There are several degrees of FPI and hypoxia:
How is intrauterine hypoxia manifested?Signs of hypoxia and their severity depend on how long the process lasts and the degree of oxygen deficiency. Alarming symptoms:
Terrible signs requiring immediate delivery:
If the violation of placental blood flow was secondary, that is, it has come due to a disease of the mother or fetus, then these pathologies appear first of all: anemia, eclampsia, renal failure. If the violation of the blood flow of the placenta is primary, then for a long time the woman does not experience any unpleasant symptoms. Sometimes you can note the frequent, erratic and intense movements of the baby. If the treatment is late, then the motor activity decreases until the complete absence of the child's tremors. It is important to remember that with chronic fetal hypoxia, symptoms may not appear until serious complications. Chronic FPI and hypoxia lead to slower fetal growth. This can be seen by the small size of the abdomen, which does not correspond to the gestational age. On ultrasound, in this case, IUGR is determined - intrauterine growth retardation of the fetus. If the fetus is smaller than it should be at a given gestational age, then it is more difficult for him to endure the difficult process of childbirth and start breathing on his own. In addition, such children often have neurological disorders and respiratory diseases. Hypoxia in childbirthDuring a normal birth, each uterine contraction (contraction) causes a temporary decrease in blood flow to the placenta. Such a short hypoxia is well tolerated by a healthy fetus, and after the uterus relaxes, the blood supply to the fetus is restored in full. If the duration of oxygen starvation during childbirth is increased, then the blood supply to the fetus is sharply disturbed. Changes begin in internal organs. If at this time the baby is not born into the world, then his death may occur at the time of childbirth or immediately after them. Causes of fetal hypoxia during childbirthSigns of fetal hypoxia during childbirth
Signs of asphyxia of the newborn (stop of oxygen supply)Hypoxia of newborns is commonly called asphyxia, and its degree (moderate or severe) is determined by the Apgar scale at the first and fifth minutes after birth. Maintaining 0-3 points on the Apgar scale for 5 minutes or more - severe asphyxia.
Signs of asphyxia of the newborn (stop of oxygen supply)Maintaining an Apgar score of 0-3 for 5 minutes or more Disorders of the brain and other organs:
Previously, it was believed that a baby could inhale the original feces (meconium) only during childbirth. Now there is evidence that in chronic hypoxia there is a risk of meconium aspiration. Moreover, the removal of the original feces from the lungs in the second case brings less results, and among the consequences there are disorders of the nervous system and frequent pneumonia.
Signs of hypoxic-ischemic encephalopathy
It is important to remember that the development of cerebral palsy in a child is often associated with hypoxia. This scenario is possible, but not required. Most children who have undergone perinatal hypoxia and do not suffer from this serious illness. Consequences of intrauterine hypoxia for a childFetal hypoxia to some extent, but almost always, is accompanied by consequences in the child after birth. The lack of oxygen in utero during the period of active growth and development of organs and systems of the fetus primarily affects the state of its nervous system and immune status. After chronic hypoxia
After acute hypoxia
All consequences for the baby are associated with brain hypoxia and premature birth, since in order to save the life of a child, emergency delivery is often used much earlier than the term. Most cases of hypoxia do not have any consequences if the child has safely survived the first month. Special methods for detecting hypoxiaIn addition to studying the anamnesis and complaints of the expectant mother, examination data and instrumental methods are used to diagnose fetal oxygen deficiency. During auscultation, the doctor listens to the fetal heart sounds, evaluates their frequency, rhythm and clarity. CTG - cardiotocographyThe purpose of the examination is to record the contractions of the baby's heart, based on the Doppler effect. Additionally, fetal movements are noted (since the heartbeat changes during movements) and contractile activity. The totality of these data helps to determine the condition of the fetus, determine its reaction to contractions and timely detect hypoxia (see). Signs of the heartbeat of a healthy fetus are:
Signs of oxygen starvation of the fetus:
During childbirth, CTG should be performed every 15 minutes, and during the pushing period - after each contraction. If signs of hypoxia appear, you can try to change the position of the body of the woman in labor to eliminate clamping of the umbilical cord. In recent years, remote CTG devices have appeared. High-risk pregnant women are offered to record a cardiotocogram at home using a special device. All results are sent via the Internet to the attending physician in real time. This allows you to quickly identify acute hypoxia and save the child. Doppler ultrasoundUsing the Doppler effect on ultrasound, you can determine the state of blood circulation in the mother-placenta-fetus system after the 20th week of pregnancy. In the study of the uterine arteries, it is possible to identify initial disorders of the uteroplacental blood flow and prevent severe fetal hypoxia. Additionally, the structure of the placenta itself and the level of amniotic waters are determined. Counting fetal movementsThis diagnostic method is rather inaccurate, therefore it is used mainly in low-risk pregnant women (without chronic maternal diseases, fetal malformations and placental pathologies). It allows you to timely identify the first stages of hypoxia, when the child changes his motor activity in response to oxygen starvation. To conduct the test, you need to get comfortable (preferably on your side) and concentrate on the movements of the baby. If less than 10 perceptible movements occur in an hour, you should immediately consult a doctor. Gynecological examinationAn examination on a gynecological chair is indicated in case of complaints of a pregnant woman about unusual discharge from the genital tract:
Analysis of blood taken from the presenting part of the fetusThis study is new and is based on determining the concentration of lactate (lactic acid) in the blood of the unborn baby. The study is possible only when the fetal bladder is opened and the cervix is dilated by 2 cm or more. Interpretation of results:
How to determine the biophysical profile of the fetusThe method includes an assessment of five main parameters of fetal health. It is carried out during high-risk pregnancy, when there is a high probability of suffering or even intrauterine death of the fetus. Respiratory rateWith a 30-minute ultrasound, the number of episodes of respiratory movements is counted. 2 points are given for a 30-second episode per half hour of observation. The absence of respiratory movements means 0 points. KTGEvaluation of the parameters of a 20-minute cardiotocographic study. If during this time 2 or more episodes of increased heart rate were observed, then the test is estimated at 2 points, the prognosis is favorable. With a "bad" CTG, the test is evaluated at 0 points. Fetal muscle toneEpisodes of limb flexion are assessed in 30 minutes. If 2 or more episodes - 2 points, if the limbs are all the time in an extended state - 0 points. Physical activityIf 3 or more active fetal movements are noted on a 30-minute ultrasound, then 2 points are given for the test. If less than 3, then the score is 2 points. If there is no movement - 0 points. amniotic fluidWith an amniotic fluid index of more than five, 2 points are put. With a lower IAI, the test is rated at 0 points. To assess the biophysical profile of the baby, scores are calculated for all 5 tests. If the sum is equal to 8-10 points, then the condition of the fetus is good, you can repeat the study after 3-4 days. If the total is less than 8 points, then additional examinations are needed, and sometimes emergency delivery. Profile evaluation is carried out twice a week. This allows timely detection of acute and chronic intrauterine hypoxia. Often the full method is replaced by an abbreviated one: only CTG and the level of amniotic fluid are evaluated. Treatment of intrauterine hypoxiaWith fetal hypoxia, treatment directly depends on the duration of pregnancy, the condition of the mother and child, and concomitant diseases of the pregnant woman. There is still no clear algorithm for eliminating oxygen starvation, since its causes are very diverse. If the patient's condition allows, the doctor may try conservative methods.
Due to the difficulties in treating fetal hypoxia, it is important to correctly plan your pregnancy, get rid of bad habits and monitor your health. After all, it is always easier to prevent and prevent a disease than to get rid of it. PreventionHow can a future mother avoid the occurrence of hypoxia in the fetus? The following recommendations will help prevent the development of this condition in the fetus:
Prevention of hypoxia in childbirth lies in the optimal method of delivery and proper management of childbirth. Question answerI have a period of 34 weeks, the gynecologist says that the pregnancy is proceeding normally, according to ultrasound, everything is also normal. But recently (about a week) I began to notice that the child moves very often, which makes me uncomfortable. Is this a sign of hypoxia?No, not at all. Many factors affect the motor activity of the fetus (mother's stress, fear, hunger, stale air in the room, and others). And in the third trimester, the size of the baby is already significant and it becomes somewhat cramped in the stomach, so most of the movements can be felt by the mother painfully. It is possible that lately you have been very nervous, thinking about the upcoming birth and neglecting a healthy lifestyle. Try to walk in the fresh air more often, stick to fractional meals (4-5 times a day), avoid feeling hungry and ventilate the bedroom before going to bed. Of course, it is worth visiting an obstetrician-gynecologist unscheduled, who will listen to the fetal heartbeat and, if necessary, prescribe a CTG. Can I listen to the fetal heartbeat on my own?Obstetricians use a special (wooden) obstetric stethoscope to listen to the heartbeats of the unborn baby. It is impossible to listen to the fetal heartbeat in this way on your own. But you can purchase a portable fetal doppler (such an ultrasound device equipped with headphones, similar in principle to a CTG machine) with which you can monitor the fetal heartbeat at home. Does it make sense to use oxygen cocktails during fetal hypoxia?Currently, oxygen cocktails are very popular, they are prescribed to pregnant women not only when any obstetric pathology is detected (anemia, early toxicosis, fetal hypoxia), but also to strengthen the immune system and saturate the body with vitamins. Oxygen cocktails are prepared from natural juices and herbal decoctions and saturated with oxygen using an oxygen mixer or cocktail and an oxygen cylinder. It is useful for expectant mothers to drink oxygen cocktails simply to prevent possible complications of pregnancy. But there are contraindications to taking such cocktails, so you should first consult with your doctor. |