By achieving success and winning life victories, you can become a victim ...

The degree of vaginal prolapse.


Conservative therapy.
Exercises lying on your back.
Kegel exercises.
Postoperative period.






At this time, you cannot:






Vaginal prolapse, or prolapse of the vaginal walls, is a complex pathological process. It is most often observed in women who have given birth after 50 years. The prevalence between the ages of 30 and 45 is 40%, up to 30 years 10%. In some cases, the disease manifests itself at a young age, even in nulliparous women.

This pathology is possible due to the weakening of the pelvic floor muscles. As a result, both the anterior and posterior walls of the vagina can fall out. If the anterior wall descends, the urethra and bladder are displaced at the same time. With pathological prolapse of the posterior wall, there is a displacement, and in more severe cases, prolapse of the rectum.
The muscles and tendons of the vagina are involved in the period of conception, during gestation, and during childbirth. And the physiological course of pregnancy and the period of childbirth depends on the state in which they are.
When carrying a pregnancy, the muscle layer of the vagina is hypertrophied, and increased tissue hyperplasia occurs. This contributes to the transfer of special elasticity to the muscle fibers. This has a beneficial effect on the biomechanism of childbirth, in which the vagina acts as a birth canal.
How to get rid of a female disease? Irina Kravtsova shared her story of recovering from thrush in 14 days. In her blog, she told what drugs she was taking, whether traditional medicine was effective, what helped and what did not.
Read the story here.
The passage of a newborn through the birth canal directly depends on the muscular state of the vaginal walls.
This pathological condition is not one-time, it develops over a long time. This is due to an increase in the pressure of internal organs (body of the uterus, bladder, rectum) on the pelvic area. The result of this long process is the prolapse of the walls of the vagina, sometimes their complete prolapse.
This disease can be accompanied by, and become the cause of the development, the following abnormal conditions:
Most often, the anterior wall descends. Falling or falling of both walls is rare.
In the development of this process, it is customary to distinguish 3 degrees of the disease:
If pressure is carried out by the displaced bladder, it leads to cystocele disease. Less commonly, rectocele occurs, which leads to a displacement of the posterior wall of the vagina.
Stories from our readers!
“The gynecologist advised me to take natural remedies. We opted for one drug - which helped to cope with hot flashes. It’s such a nightmare that sometimes you don’t even want to leave your home for work, but you have to ... As the appointment began, it became much easier, you even feel that some kind of inner energy has appeared. And I even wanted to have a sexual relationship with my husband again, otherwise it was all without much desire. "
The development of this pathological process can occur over several decades. And only sometimes, due to difficult childbirth or improper obstetrics, the process can be more rapid.
The patient may feel the first symptoms in the form of pain during intercourse.
As the disease progresses, the following symptoms appear:
At an early stage, a woman does not go to a doctor because she is not worried about anything. However, with a vaginal examination, which is carried out during a prophylactic examination, the gynecologist may see a slight sagging of the vaginal wall.
Later periods lead to the development of a hernial protrusion. In this process, the vaginal wall is a hernial sac, and contains a portion of the bladder.
A similar clinical picture can develop with the back wall of the vagina. With such a development of pathology, a part of the rectum will appear in the hernial sac.
To make the correct diagnosis, in most cases, the gynecologist only needs to make a preliminary examination using a vaginal speculum, as well as a palpation examination.
After carrying out these measures, the organs that have fallen out are repositioned, along the way, the condition of the muscles of the pelvic floor is assessed. Additional examination methods are prescribed by a doctor.
Premenstrual pain and unpleasant discharge are over!
Our reader Egorova M.A. shared her experience:

It is scary when women do not know the true cause of their diseases, because problems with the menstrual cycle can be harbingers of serious gynecological diseases!
The norm is a cycle lasting 21-35 days (usually 28 days), accompanied by menstruation lasting 3-7 days with moderate blood loss without clots. Alas, the state of gynecological health of our women is simply catastrophic, every second woman has some kind of problems.
Today we will talk about a new natural remedy that kills pathogenic bacteria and infections, restores immunity, which simply restarts the body and turns on the regeneration of damaged cells and eliminates the cause of disease ...
At the onset of pregnancy, even in a healthy woman, the musculo-ligamentous apparatus is subjected to great stress. This is due to the growth of the fetus. In the case when the patient is diagnosed with prolapse of the vaginal walls, a favorable pregnancy outcome is possible only at the initial stage.
At the same time, throughout the entire gestation period, it is necessary to use the Kegel complex of therapeutic gymnastics, be sure to wear a bandage, or use a pessary (this is a plastic ring that is inserted into the vagina and increases its muscle tone).
Treatment features:
To avoid this pathology, it is enough to show up for an appointment with a gynecologist once every six months, and without his appointment to engage in therapeutic exercises every morning.
To choose the right tactics for treating this disease, its degree is established. This can only be done by a doctor.
If this pathology is at the first degree of the disease, then the patient can be treated with a conservative method of therapy. At the third or fourth degree, the main tactic of treatment is surgical intervention, followed by preventive measures.
This technique involves a set of measures to increase muscle tone. For this purpose, it is appointed:
The complex of therapeutic exercises is selected individually, you need to do it daily, preferably in the morning before breakfast.
To carry it out, you can use the following exercises:
The entire set of exercises should begin with a minimum amount of time and repetitions, and the increase in load should be done gradually.
For its implementation, a gynecological chair is used. With one hand, the gynecologist performs massage actions, inserting two fingers into the lumen of the vagina, the other hand, performs massage movements along the anterior abdominal wall.
The number of sessions should be at least 10, after which a short break is taken and a second course of massage takes place.
DID YOU KNOW? The disadvantage of most drugs is side effects. Often drugs cause severe intoxication, subsequently causing complications of the kidneys and liver. To prevent the side effects of such drugs, we want to pay attention to special phytotampons. Read more here.
A prerequisite for the entire course, the patient should sleep only on her stomach. The session lasts no more than 15 minutes; when severe pain appears, it is no longer prescribed.
Bandage is a special swimming trunks with a high waist. Highly elastic jersey is used in their manufacture. Modern versions of this product make it invisible under clothes. With the help of special hooks located on the side, the degree of its tension is adjusted.
With the correct choice of tension, it does not hinder movement, is comfortable to wear and hygienic.
A pessary can be used to prevent sagging of the vaginal walls. These products are made of plastic or silicone and come in various shapes, most often in the form of a ring. The shape and size is selected by the gynecologist, individually, taking into account the physiological characteristics of the patient.
It is very important that the gynecologist installs the pessary for the first time.
After 2 weeks of wearing the pessary, you need to see a specialist. It can be worn for no more than 1 month, after which a short break is taken. It is imperative to treat with an antiseptic with each subsequent introduction.
Correct use of the uterine ring will allow:
Particular attention must be paid to the correct diet. The food consumed should not lead to increased gas production in the intestines. It is also necessary to avoid constipation.
This requires:
Therapy with medicinal herbs, with the help of which infusions of decoctions are made, gives a positive effect only at the initial stage of this pathological process. The use of traditional medicine recipes cannot be the main type of treatment; it is used as an additional method. In this case, the use of medicinal herbs should be agreed with the gynecologist.
To raise muscle tone and strengthen ligaments, you can use:
If conservative treatment has not led to the appearance of positive results, or this pathology is at the level of 3 or 4 stages of its development. This provides the basis for an operable treatment technique for this abnormal development.
Surgical intervention can be carried out using 2 methods:
Surgical intervention can consist of two stages. With an additional stage, the internal organs are sutured, which exert excessive pressure (due to their prolapse) on the vaginal walls.
This makes it possible to restore the anatomical location of these organs, after which they will restore their physiological functions.
Front wall pulling is carried out through the lumen of the vagina, this avoids the incision of the abdominal wall. As a result, the surgical intervention becomes less traumatic, it brings a little psycho-emotional discomfort to the sick woman.
Before surgery, women of advanced age, especially during menopause, are prescribed hormones. They increase blood circulation and normalize the process of tissue repair after surgery.
During the rehabilitation period, antibiotic therapy is prescribed, drugs of the analgesic group. The patient is given recommendations, including warn her about abstaining from sexual intercourse.
Its main purpose is to restore the septum between the rectum and the vaginal wall. The group of muscles holding the anus is sutured. This leads to a strengthening of the rectovaginal septum. If necessary, the removal (if any) of hemorrhoids, polypous outgrowths, treatment of the fissure of the anus and the sphincter of the anus occurs.
This type of operation is rarely used, since it removes the consequences of prolapse, only temporarily. But if it is used in combination with colporrhaphy, then it gives a good positive dynamics in the treatment of this pathology.
The essence of this operable treatment is that the weakened vaginal walls are sutured to the ligaments and fascia of the inner walls of the abdomen. This type of surgical intervention has received a "second life" due to the use of advanced technologies in medicine and the use of new materials (polypropylene mesh is used).
The recovery period can last from 5 to 20 days. It depends on the technique used during the surgery.
Patients are assigned:
When discharged from the hospital, a woman is given a number of recommendations that she must follow in order to prevent the re-development of the pathological condition:
During the rehabilitation period, the use of physical activity is not allowed, but after 2 or 3 months, the doctor prescribes therapeutic exercises. It should be dosed, and you should start using it gradually (records are not needed in this case).
You can use different types of exercises, of which make up a complex that will be carried out daily in the morning.
To do this, you can use the following exercises on all fours:
Exercises lying on your back:
All exercises are performed in slow motion, with mandatory breathing control. This is best done 2 hours before meals (before breakfast).
The main Kegel exercises include:
Preventive measures to eliminate this pathology should be carried out upon reaching the age of 18 years. This will contribute to the normal course of pregnancy and the smooth passage of labor.
To do this, you must observe the following rules:
Medical professionals play an important role in the prevention of this pathology.
Since it depends on them:
This pathology can lead to the development of serious gynecological diseases. Therefore, in order to eliminate the prolapse of the vaginal walls, in the early stages, use all possible conservative methods of treatment.
In the event that the disease was recognized only at a later date, agree on the date of the operation with the doctor, and do not postpone its implementation.
The downside of most drugs, including those described in this article, is side effects. Often, medications are very harmful to the body, subsequently causing complications in the work of the kidneys and liver.
To prevent the side effects of such preparations, we would like to draw your attention to the special phytotampons BEAUTIFUL LIFE.
They contain natural medicinal herbs - this gives tremendous effects of cleansing the body and restoring women's health.
Read more about how this drug helped other women here in our article on phytotampons.
We wish you good health!
Obstetrician-gynecologist of the highest category and author of articles woman-centre.com. For more than 20 years she has been successfully helping women to get treatment for gynecological diseases.
Prolapse of the vaginal walls or vaginal prolapse is an abnormal condition in the female reproductive system that mainly occurs in women who have given birth after fifty years due to a weakening of the pelvic floor, but it can also occur in women aged 30 to 45 years (forty cases out of a hundred) , as well as up to thirty years (ten cases out of a hundred). Vaginal prolapse is not always associated with childbirth; in three percent of cases, an abnormal condition develops in young and nulliparous girls.

Causes or mechanism of vaginal prolapse. Prolapse of the vaginal walls (prolapse) is expressed in a change in the anatomical location of the pelvic organs against the background of weakening of the muscles of the abdominal region and pelvic floor. Why is this happening? Due to the increase in pressure inside the abdominal region, the elasticity of the ligaments is gradually lost, because of which they are unable to keep the internal organs (in particular, the bladder, uterus, rectum) in the required physiological position. Hence, an increase in organ pressure gradually leads to a loss of muscle tone in the perineum and prolapse of the tissues of the vagina.
Many factors can contribute to the development of such a condition, including:
The process of the course of the disease is characterized by a slow pace at the beginning and rapid progression in the future, often accompanied by diseases of an inflammatory nature.
In the course of the development of the disease, either the anterior or the posterior wall of the vagina can undergo prolapse, or both can be simultaneously. In clinical practice, the prolapse of the anterior wall is most common, which is inevitably accompanied by a prolapse of the bladder and urethra. When the posterior wall of the vagina descends, there is a high risk of prolapse or prolapse of the rectum.
The degree of vaginal prolapse.


Signs of prolapse and prolapse of the vaginal walls. In the early stages of development, the disease does not manifest itself in any way. The first alarm bells signaling the disease are pain during sexual intercourse and a weakening of sensations during this process. Further, heaviness and pressure in the vulva may be felt, as the progression, inflammation, swelling of the genital gap, discomfort during urination, incontinence (urine, stool and gas), pulling pains in the abdomen, lumbar region join.
The prolapse of the anterior wall of the vagina most often manifests itself in the form of the development of chronic cystitis against the background of stagnation of urine, the posterior wall - in the form of constipation and a feeling of the presence of a foreign object in the vulva.
A complication of the prolapse of any of the walls of the vagina is often prolapse, and then prolapse of the uterus, which manifests itself in the form of excessive blood or bloody discharge.
Diagnosis of prolapse and prolapse of the vaginal walls. Identifying the disease is not difficult; when examined in a gynecological chair, the walls of the vagina and cervix protruding from the genital tract are noticeable. The doctor adjusts them, and then evaluates the condition of the pelvic floor muscles. In this case, an additional consultation with a urologist and a proctologist is mandatory.
Prolapse of the vaginal walls and pregnancy. Pregnancy with this condition is possible, but the degree of development of the disease should be taken into account. The first degree of the disease allows you to give birth without a preliminary operation. In this case, exercises to strengthen the pelvic muscles and the press will help. With a progressive degree of the disease, surgery, recovery is necessary, only then can you become pregnant. Otherwise, prolapse of the vagina is fraught with prolapse of the uterus.
Treatment of prolapse of the vaginal walls. The prolapse of the vaginal walls, subject to early diagnosis, can be eliminated conservatively; in more advanced and complicated cases, surgical intervention is performed. Timely treatment significantly reduces the risk of complications.
Conservative therapy. Therapy is indicated for insignificant prolapse of the vaginal walls and is expressed in the use of a set of exercises, the purpose of which is to increase the muscle tone of the pelvic floor, including Kegel exercises (compression and relaxation of the muscles of the perineum), physical therapy. At the same time, therapy is prescribed for the general strengthening of the body, while nutrition is not of the last importance (no heavy foods that can cause constipation and complicate the problem).
During menopause, women are shown hormone replacement therapy in order to improve blood circulation and strengthen the muscles and ligaments of the pelvic organs.
If an operation is contraindicated for a woman for any reason, to prevent complete prolapse of the uterus, the patient is fitted with uterine rings (pessaries) - a device to support the internal organs is inserted into the vulva. The pessary is selected for each patient individually, after which regular observation by the gynecologist is shown, in order to exclude the development of serious complications (processes of a purulent and ulcerative nature, irritation and swelling of the mucous membrane, ingrowth of the pessary into the cervix or vulva). To prevent these phenomena, the doctor prescribes douching and washing the vagina. If the weakness of the vaginal muscles does not allow the introduction of the pessary, then a hysterophore is used - a device that holds the uterus through a pessary connected to a bandage attached to the waist.
Gymnastics (a set of exercises) with the lowering of the walls of the vagina at an early stage (can be used as a prophylaxis of the disease).
Exercises on all fours:
Exercises lying on your back.
Exercise should be done slowly and with control of your breathing. Do it two hours before meals or two hours later. The time for classes is not limited.
Kegel exercises.
Surgery for prolapse and prolapse of the vaginal walls (plastic of the vaginal walls). After examining the patient with the participation of a proctologist and urologist, the doctor prescribes treatment, taking into account the severity of the pathology, the degree of loss, the patient's age and the individual characteristics of her body. As a rule, surgical treatment with plastic elements is recommended. This is mainly colpoplasty, which involves suturing the vaginal walls. There are two types of colpoplasty:
Surgical intervention is carried out using general anesthesia. The choice of the procedure for the operation is determined by the surgeon, taking into account the visual and video colposcopic examination, the analysis of the condition of the tissues of the walls of the vulva and the presence of concomitant diseases of the pelvic organs.
Postoperative period. After assessing the general condition of the patient after the intervention, the doctor discharges her, usually on the second day after the intervention. To prevent the development of complications and accelerate the recovery period, it is necessary to strictly follow all the doctor's recommendations, namely:
Modern equipment and microsurgery capabilities make it possible to carry out an operation with low trauma. After the intervention, there are no visible traces and scars on the body.
Prevention of prolapse of the vaginal walls.
Treatment of prolapse of the vaginal walls with folk remedies. Treatment with traditional medicine can only have an effect at an early stage and in combination with other therapies prescribed by a doctor, including exercise.
Quince can be brewed and drunk in the form of tea, it gives tone to the muscles of the uterus. For 100 g of dried fruits and a liter of water, brew in a water bath.
Alcohol tincture of astragalus root is also considered an effective traditional medicine against this ailment. For a part of the chopped roots, take nine parts of vodka. Keep the mixture in a cool, dark place for two weeks. Then strain. Take three times before the main meal (breakfast, lunch, dinner) with plenty of water. The treatment course includes thirty days, if necessary, the course can be repeated after two weeks.
Mix 50 g of lime blossom and lemon balm each, add 70 g of white ash and 10 g of alder root. Grind the mixture. Take two tablespoons, boil 200 ml of boiling water and insist until it cools completely. Take half a glass three times daily before meals. The course of treatment is twenty-one days, after two weeks of a break, the course can be repeated.
Datura is effective as a sitz bath for partial drooping. Pour 20 g of grass with seven liters of boiling water and keep in a water bath for fifteen minutes. After that, the infusion should be cooled to 38 degrees. Use for a sitz bath, which lasts no more than ten minutes.
What to do with vaginal prolapse?
What to do with vaginal prolapse? At the first degree of pathology, it is possible to use conservative methods of treatment. These include: exercise, gynecological massage, and herbs. All of these methods are needed to increase the tone of the pelvic muscles and reduce the likelihood of vaginal prolapse.
There is another method of dealing with vaginal prolapse - a pessary, or otherwise - the uterine ring. It is located in the vagina, which helps to keep the cervix in a physiological position.
As a result, the uterus is in a slightly elevated state, since the pessary covers the cervix and holds the entire organ. It is rational to use such a ring with slight omission or in old age, with the expectation that age-related changes contribute to a decrease in organs in size and mass.
The disadvantage of a pessary is the need for frequent washing, as well as individual selection in volume. In addition, the use of a bandage is considered mandatory, which also supports the pelvic organs.
Vaginal prolapse treatment
The tactics of treatment are determined by the degree of development of the pathology, the age of the woman and the presence of concomitant diseases. It is customary to distinguish two directions in treatment - the conservative way and the operative one.
Conservative treatment of vaginal prolapse is used for the 1st degree of prolapse, when the structures of the vagina do not cross the border of the genital slit. It consists in limiting physical activity, lifting weights, conducting a course of gynecological massage, as well as performing special physical exercises.
Vaginal prolapse treatment focuses on strengthening the pelvic muscles, supporting structures and abdominal muscles, which keep the internal organs in their physiological position. In addition, in the process of massage and exercise, blood circulation in the pelvis is activated, which is also necessary for treatment.
Vaginal prolapse surgery
A method of treating pathology - an operation for prolapse of the vagina consists in carrying out colpoplasty, the essence of which is based on suturing the walls of the vagina. This type of surgical intervention is of two types: colporrhaphy and colpoperineorrhaphy.
The first form of surgery involves resection (excision) of the tissues of the vaginal walls, which are "stretched" with further stitching of the remaining structures. In the process of colpoperineorrhaphy, a decrease in the size of the posterior wall is carried out by suturing it, as well as a tightening of the pelvic muscles.
Vaginal prolapse surgery may involve an additional step involving the surrounding internal organs such as the bladder, urethra and rectum. To reduce the manifestation of symptoms of dysfunction of these organs, it is necessary to restore their physiological location.
Plastic surgery can take place with your own tissues or using implants. Surgery is performed under general or epidural anesthesia. The choice is based on the scope of the proposed operation, its duration and the state of health of the woman.
Surgery for lowering the anterior vaginal wall
In order to tighten the organs, ensuring their physiological location, and prevent the formation of new defects that can provoke a relapse, an operation is used when the anterior vaginal wall is pushed down.
In addition, surgery improves a woman's sexual performance and is used to treat urinary incontinence.
Surgery for lowering the anterior vaginal wall is called anterior colporrhaphy. Modern equipment provides the use of vaginal access, which is less traumatic than laparoscopy and access through the abdominal cavity.
The preparatory period before surgery includes the use of hormonal agents, especially for women in menopause. They are necessary to improve local blood circulation, which has a positive effect on the postoperative recovery period.
After surgery, it is necessary to use antibacterial drugs to prevent infection of the operated lesion, as well as pain relievers, with the exception of aspirin. In addition, it is recommended to abstain from sexual activity for at least a month.
Surgery for lowering the posterior wall of the vagina
An operation is performed when the posterior wall of the vagina is lowered for resection of the intestine, which protrudes towards the vagina and exerts pressure on its posterior wall, and in order to restore the rectovaginal septum.
Surgical intervention consists in eliminating intestinal protrusion, strengthening the wall (anterior) of the rectum, the septum between the intestine and the vagina, as well as in normalizing the function of the sphincter of the anus.
Surgery for lowering the posterior wall of the vagina involves suturing the intestinal wall with a group of muscles that raise the anus, which helps to strengthen the septum between the organs.
In the presence of concomitant pathology and involvement of the surrounding organs in the pathological process, the volume of surgical intervention increases to eliminate the physiological location of the structures.
So, a combination of the main direction of the operation with the treatment of prolapse of the anterior vaginal wall, hemorrhoids, polyposis formations or anus fissures is possible. As a result, the time of surgical intervention is increased. In addition, in some cases, endoscopic treatment with a mesh implant is allowed.
Exercises for lowering the vagina
The close connection of the vagina with the uterus predisposes to their joint prolapse, first the vagina, and then the uterus. Exercises for lowering the vagina have a strengthening effect on the muscles, with the help of which the organs maintain their physiological position.
The maximum result can be obtained when using these exercises at the initial stage of vaginal prolapse, since in addition to it, the surrounding structures are not yet involved in the pathological process.
The simplest exercise to exercise is to stop urinating by tightening the muscles. Stopping the jet from time to time during urination will help strengthen the muscles and combat urinary incontinence.
Vaginal prolapse exercises should be done at different rates throughout the day. Of course, you should not constantly train, but 3-4 times a day, several exercises will help to normalize muscle tone soon.
The workout can be done while sitting at the computer, standing at a bus stop, or at home in the "lying" and "standing on all fours" positions.
Kegel exercises for lowering the vagina
Before you start doing the exercises, you need to determine which muscles will have to work and where they are. To do this, during urination, try to stop the stream and remember how this is done. These muscles will have to be trained in the future.
Kegel exercises for lowering the vagina include 3 types of performance. Firstly, this is the contraction of those very detected muscles. However, the execution should be slow, squeezing the muscles you need to count to 3 and slowly relax them.
After that, you need to do the same thing, only quickly. And, finally, "pushing out" is performed by tension of the abdominal muscles, as in childbirth, but much weaker.
In order to control the correctness of the exercise, it is recommended to insert a finger into the vagina and monitor the contractions.
First, you need to start with 10 times of each exercise, performing 5 times a day, and then gradually increase the load. After a week, add 5 repetitions to each exercise, and so on until you get 30 times. To maintain the effect, you can stop at this load and perform these 3 exercises 30 times 5 times a day.
Bandage for lowering the vagina
The prolapse of organs occurs due to the loss of the muscular frame that supports them. So, after pregnancy and childbirth, muscle relaxation is most often observed to such an extent that vaginal prolapse is possible.
A bandage for lowering the vagina is necessary in order to maintain constant intra-abdominal pressure without lifting, which affects the location of the uterus and vagina. The bandage gives the muscles time to restore their tone and strengthen the organs in physiological positions.
Although effective, the vaginal lowering band should not be used continuously as the organs need rest. So, at night it is not rational to use it, since neither gravity nor pressure contribute to the prolapse of the vagina.
During even little physical activity (walking, doing housework), you must wear a bandage to support the organs. In addition, it is mandatory after operations on the uterus and vagina, since the muscles in the postoperative period are the weakest and are not able to perform the main function.
Folk remedies for vaginal prolapse
For the purpose of treating a pathological condition, it is recommended to simultaneously use physical exercises and folk remedies for prolapse of the vagina. For this, a collection of herbs is used, taken orally, in the form of baths or douching.
For the broth, you need to take lemon balm and linden flowers - a quarter of a glass each, white lamb - 70 g and alder root - 1 dessert spoon. After thorough grinding, you need to select 30 g of the mixture and pour boiling water in a volume of one glass.
The broth should be infused for about 1 hour, after which it should be filtered and taken in 100 ml three times a day before meals for half an hour. The duration of the course is 20 days, and then a break is needed - half a month.
For douching, you will need to prepare a solution from quince, which must be crushed and filled with water, the volume of which is 10 times the quince. After boiling for 25 minutes, the broth should be filtered and cooled to a warm comfortable temperature. Douching with this solution helps to increase muscle tone.
Exercise therapy for vaginal prolapse
Exercises should be repeated every morning before meals, starting with the minimum load and gradually increasing it. Exercise therapy during vaginal prolapse helps to restore the previous muscle tone and strengthen them for a longer time.
"Bicycle" is an exercise that has been familiar to everyone for a long time. To perform it, it is enough to lie down and pedal an imaginary bicycle for about a minute, raising your legs 45 °. In the same way, "scissors" are performed, but with straight legs.
Lie on the floor, put a twisted roller under the buttocks, while the back remains on the floor. The left leg must be lifted straight up to 90 °, and then lowered and changed to another. Repeat up to 8-12 times.
The exercise becomes more difficult, removing the roller, you should simultaneously raise both legs to an angle perpendicular to the floor. Standing near a chair, you need to stick to it and take your leg to the side in order to perform circular movements for 30 seconds. Then change direction and then leg. Also, while standing, you need to swing your leg up to 7 times each, stand in the "swallow" pose - for about a minute.
Vaginal prolapse can bother women at any age, but there is an effective way to prevent muscle weakening - this is physical exercise, so if you want to, you can independently reduce the chances of developing pathology.
Feelings of an unpleasant nature in the vagina during physical exertion, compression of the pelvic floor muscles, and intimate life are a reason for a woman to consult a specialist. The problem may lie in the displacement of the body of the uterus and fraught with serious consequences and a threat to the health of a woman.

The body of the uterus is displaced unevenly, the back or front surface descends downward. The process of lowering the posterior wall of the vagina, in which there is pressure on the rectum, is called rectocele. The early stage of this disease is almost asymptomatic.

The first thing that a woman begins to feel is pain during sex. For the disease in later stages, the following symptoms are characteristic:

At the last stage, a woman can no longer have sex. Simultaneously with the prolapse of the body of the uterus, erosion and other inflammatory processes occur.
The method of treating rectocele depends on the degree of prolapse; for this, ultrasound studies, urography, colposcopy are prescribed, laboratory tests are taken, smears and feces are examined.
Prolapse of the uterus is a serious disease, ignoring which always leads to irreversible consequences.
Early diagnosis will allow you to get rid of this problem at the first stage and avoid unpleasant consequences. What to do if a descent of the back wall is diagnosed with moisture, this disease is treated with an operative method, laser correction or conservative treatment.
Laser correction is a modern non-surgical method using modern technologies. This is the safest and most effective treatment for rejuvenating and restoring the turgor of the vaginal walls.
Surgical intervention is performed at 2 and 3 stages of displacement. During a surgical operation, surfaces are tightened and sutured, implants are implanted to fix organs. In addition to the above methods of treatment for vaginal prolapse, drug therapy is prescribed, as well as a gymnastic complex.
If the treatment of prolapse was not started on time, with advanced stages, the only way to eliminate organ prolapse is to use a surgical scalpel. Modern surgery offers women diagnosed with prolapse of the back wall moisture to perform an operation and at the same time plastic surgery. This type of colpoplasty is called posterior colporrhaphy.
The purpose of the operation is to remove excess tissue, narrow the vaginal opening, and restore the anatomical location of organs.
This surgery has its own characteristics. The surgeon needs to remove the extra tissue flap on the vaginal wall adjacent to the perineum. The size of the cut fabric should be such that the seams do not come apart after overstraining.
The first 3 - 4 days, patients are assigned to bed rest, the woman is under the supervision of a doctor in a hospital. The rehabilitation period after colporrhaphy lasts 1.5 months. At this time, you cannot:
Among the contraindications for colporrhaphy are venereal diseases, heart disease, acute stages of thrombophlebitis.
In milder forms of prolapse, the following help to restore the anatomical location of organs:
A woman who uses corrective rings must wear a bandage, observe the strictest hygiene and see a doctor.
A strict diet of plant fiber also helps. Foods with a high percentage of fiber help the easy passage of feces through the intestines. It is recommended to take laxatives and eubiotics that restore the intestinal microflora.
Along with diet, pharmaceuticals and physical therapy, it is recommended to use recipes from traditional medicine to help increase muscle tone. These are douching and baths with quince solution, decoctions inside from lemon balm, alder, linden color, white ash.
It is necessary to wear a supportive bandage for rectocele, especially for women after childbirth, when muscle tone is weakened. You cannot wear the device all the time, the body must get rest.
Physiotherapy exercises and special Kegel exercises will help restore the anatomical positions of organs and strengthen muscle tone. Exercise therapy is carried out at the first stage under the supervision of an instructor; in the future, a woman can perform a simple gymnastic complex on her own.
Exercises allow you to get the greatest therapeutic effect:
The Kegel complex is effective for genital prolapse. These are three simple but effective exercises: stepped tension and such relaxation of the pelvic muscles, delaying the stream during urination for a few seconds and moderate attempts, as in labor.
Specialists in aesthetic gynecology are successfully dealing with the problem of restoring the tone of the muscular structures of the vagina. Laser correction is performed using special medical equipment and takes up to 30 minutes. This non-invasive treatment is performed with a laser beam. With the help of a laser, excess tissue is heated and evaporated. Such technologies contribute to better regeneration, increased blood circulation, and the production of collagen fibers.
After the laser procedure, normal turgor is restored, the tissues acquire elasticity, and the volume of the vagina decreases. Discomfort disappears, the normal process of urination is restored.
The cost of laser therapy in aesthetic gynecology clinics depends on the degree of wall prolapse:
The prolapse of internal organs is a serious pathology, it is dangerous with unique consequences. The sooner the disease is diagnosed, the faster it can be cured.
Treatment of prolapse of the vaginal walls according to the recipes of the newspaper "Vestnik HLS".
Kegel exercises can help you do without surgery
A 47-year-old woman turned to the newspaper: she was diagnosed with prolapse of the vaginal walls, and an operation was proposed. But she is afraid to go under the knife. I heard that exercises help to cope with this problem. Asks for information on these exercises.
The doctor-gynecologist A. I. Shashina is in charge. The main reasons for the prolapse of the vaginal walls are prolonged leg work or work associated with lifting weights. These two reasons in 99% of cases will lead to the development of this disease. Therefore, first of all, a woman needs to reconsider her lifestyle, change her job.
The exercises that the reader writes about were developed by the German gynecologist Arnold Kegel. They strengthen the pelvic floor very well.
These are the exercises.
1. First you need to learn how to compress and unclench the muscles of the perineum. Tighten them as if you are trying to stop urination. Hold the muscles in this state for 3 seconds. Relax.
2. The same exercise, but at a fast pace - quickly contract and relax these muscles.
3. Squeeze the muscles of the perineum and stay in this position as long as possible - 1-1.5 minutes.
4. Imagine that you need to push something out of the muscles of the perineum. Tighten your muscles (push) with medium strength. Try to hold this position longer.
Kegel exercises can be performed in any position, it does not matter of fundamental importance, even sitting, even lying down, even standing. If only the woman herself was comfortable doing them.
For the first week, do each exercise 10 times, 3-5 sets per day.
In the second week - 15 repetitions.
In the third week - 20 repetitions.
So keep increasing the number of repetitions until you get to 100 times. Gradually, the pelvic floor muscles will become so strong that no surgery is needed for the prolapse of the vaginal walls.
(HLS 2015, No. 8, p. 22).
Descent perineum syndrome (prolapse of the vaginal walls, prolapse of the uterus) Is a very common occurrence. However, many simply think that this is a variant of the norm, one can live with it, and, most importantly, that I'm ashamed to say about it! They just get used to this state.
Indeed, at the initial stages, nothing worries. Only during sexual activity do sensations change (the vagina becomes wider). Over time, complaints of urinary incontinence join, chronic inflammatory diseases of the vagina, cystitis, pathological discharge from the genital tract occur. Long-term conservative treatment does not bring the desired result.
And everything is connected with the fact that the walls of the vagina go beyond the boundaries of the genital crevice, constantly in contact with the underwear and the rectal area.
The main reasons that lead women to see a doctor are as follows:
Let's try to explain a little what is happening and what leads to such a change in anatomy:
The reasons for the prolapse and prolapse of the female genital organs (prolapse of the walls of the vagina, prolapse and prolapse of the uterus) are as follows:
In both the first and second cases, there is a weakening of the interconnections between the muscles of the pelvic floor, they weaken and cease to support the pelvic organs from below. This leads to the fact that the walls of the vagina begin to gradually descend from top to bottom (omission of the walls of the vagina), going beyond the genital slit. Subsequently, there is a prolapse and prolapse of the uterus, which, as it were, stretches the vagina behind itself.
 The plane of the pelvic floor shifts downward, and this leads to prolapse of the pelvic organs (vagina, uterus, rectum), anal incontinence, urinary incontinence. Despite the fact that the disease is often encountered and seriously studied, the mechanism of its occurrence is practically unknown. Also, there is no unambiguous definition of the syndrome of prolapse of the perineum and a clear classification.
The plane of the pelvic floor shifts downward, and this leads to prolapse of the pelvic organs (vagina, uterus, rectum), anal incontinence, urinary incontinence. Despite the fact that the disease is often encountered and seriously studied, the mechanism of its occurrence is practically unknown. Also, there is no unambiguous definition of the syndrome of prolapse of the perineum and a clear classification.
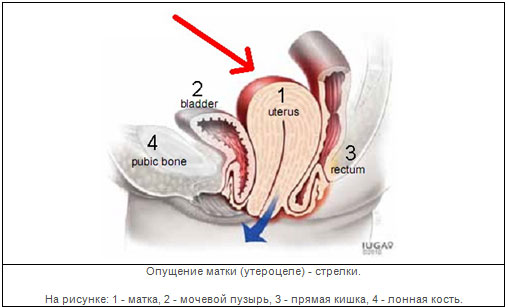
As you can see in the figure, the bladder is present in front of the vagina, and the rectum is in the back. The basis of the pelvic floor is made up of muscles, which are normally tightly spliced together in the center of the perineum.
Genital prolapse(in particular, prolapse of the uterus) is their downward displacement. The whole organ or any of its walls can be displaced.
The incidence of prolapse of the uterus and vagina is 12-30% in multiparous women and 2% in nulliparous women!
And according to the literature, the risk of undergoing surgery to correct the prolapse of the vagina and uterus during life is 11%.
In medical terms for prolapse of the genitals, there is the ending "tsele". And quite often this raises a number of questions in patients. Translated from Greek, this word means "swelling, swelling." To facilitate understanding of medical terminology, you can read
Cystocele- bulging (like a protrusion) of the posterior wall of the bladder into the lumen of the vagina.
Cystourethrocele- a combination of a cystocele with a displacement of the proximal urethra.
 Rectocele- bulging of the rectum into the lumen of the vagina.
Rectocele- bulging of the rectum into the lumen of the vagina. 
Enterocele- bulging of the loop of the small intestine into the lumen of the vagina.
The most common combination of cystocele and rectocele, which requires additional correction
The position of the pelvic organs (from prolapse of the vagina and prolapse of the uterus to its extreme degree: prolapse of the uterus) is usually assessed subjectively using a scale from 0 to 3 or from 0 to 4 points. Zero points corresponds to the norm, the highest point corresponds to complete organ prolapse. In case of prolapse, the uterus extends beyond the genital slit completely (complete prolapse) or partially, sometimes only the cervix (incomplete prolapse).
There is a classification of prolapse and prolapse of the vagina and uterus(M.S. Malinovsky)
Loss of I degree:
Loss II degree:
Loss III degree (complete loss):
The following factors can become prerequisites for the prolapse of the pelvic organs:
The problem of prolapse and prolapse of the vagina and uterus continues to be the focus of attention of gynecological surgeons, since, despite the variety of different methods of surgical treatment, relapses of the disease often occur. The solution to this problem is especially important in the treatment of patients of reproductive and working age. In the presence of minimal signs of prolapse of the vaginal walls, it is necessary to take preventive measures.
Treatment methods
In recent years, the use of synthetic prostheses, which provide additional support to the pelvic organs and prevent the development of relapses, has become of great importance in reconstructive pelvic surgery.
For the treatment of prolapse, a special polypropylene mesh GYNEMESH PS (Johnson & Johnson) is used, as well as the PROLIFT system (Johnson & Johnson) to restore the anterior, posterior sections or complete restoration of the pelvic floor. The PROLIFT system was developed by leading pelvic surgeons and is today the most modern approach for pelvic floor reconstruction in women.
The purpose of using the PROLIFT system is the complete anatomical elimination of pelvic floor defects according to a standardized technique. Depending on the localization of the defect and the surgeon's preferences, the procedure can be performed in the form of reconstruction of the anterior or posterior sections, as well as complete restoration of the pelvic floor. The essence of the intervention consists in the installation of one or two synthetic polypropylene (GYNEMESH PS) mesh implants using a vaginal approach.
These implants are placed without tension and are designed to close all existing and potential pelvic floor defects.
More than half of the cases of pelvic organ prolapse are associated with urinary incontinence.
Currently, clinicians with the TVT, GYNEMESH PS, and PROLIFT surgical techniques can combine these operations while strengthening the pelvic floor organs and eliminating stress urinary incontinence. This procedure is easily tolerated and allows the patient to return to normal life as soon as possible.
Vaginal prolapse- displacement of the female genital organ downward with the exit from the genital slit. The disease is observed more often in mature women from 40 years old, since it can be caused by a reorganization of the reproductive system, menopause, the consequences of frequent and difficult childbirth, operations on the uterus, and lifting weights.
The prolapse of one, two vaginal walls or the entire organ at once often occurs after childbirth. In women who have recently given birth, vaginal prolapse manifests itself as a feeling of heaviness in the lower abdomen due to pressing on the abdominal wall of the bladder.
But most often, the pathology does not manifest itself in any way at an early stage and is diagnosed only at an appointment with a gynecologist. At the 2nd, 3rd stage, characteristic painful symptoms (pain, urological problems) appear, which indicate that treatment should be started immediately - to do gymnastics, massage.
The vagina may fall out in whole or in part. The complete prolapse of the organ cannot be cured conservatively, and after the operation you will have to wear a bandage, therefore, at the first signs of illness after childbirth and not only, it is better to consult a doctor.
The prolapse of the vagina is divided into 2 types:
Partial (incomplete) prolapse of the vagina (prolapsus vaginae partialis) is a displacement of a part of the vaginal wall, which protrudes from the vulva in the form of a fold. The anterior, posterior wall of the vaginal canal can fall out, both at the same time. If the anterior wall is displaced, the urethra and bladder descend into the cavity of the vaginal canal. When the back wall falls out, vaginal prolapse is complicated by prolapse of the rectum.
Complete prolapse of the vagina (prolapsus vaginae totalis) - the exit of the entire vaginal tube outside the vulva. Often accompanied by prolapse of the uterus.
Since the disease develops gradually, there are 3 degrees of vaginal prolapse.
The 1st degree is characterized by the prolapse of only the walls (anterior or posterior), while the vulva remains within the limits of the boundaries allowed by the anatomy.
2nd degree - the anterior or posterior wall and part of the bladder and rectum partially descend.
3rd degree - the vagina falls out of the genital slit along with the uterus, part of the bladder, rectum.
The prolapse of the vagina has various signs that change with the development of the disease. At first (sometimes for several years), a woman feels pain during sex, discomfort in the vaginal area when straining, pulling pain, heaviness in the lower abdomen, as during menstruation, notices bloody vaginal discharge. These signs are very often absent.
The disease then progresses rapidly and symptoms become more onerous. Women feel the presence of a foreign body in the genital gap, problems with urination and defecation begin, it becomes impossible to have sex because of severe pain.
Frequent urge to go to the toilet does not bring relief, since stagnant processes begin in the bladder, a "pocket" is formed in the rectum, in which feces accumulate. Patients begin to suffer from involuntary urination, gas incontinence, constipation.
With partial and complete prolapse, the structure of the vaginal mucosa is disturbed, it becomes vulnerable to infections. Against the background of vaginal prolapse, inflammatory, erosive processes (for example, cystitis) develop.
The prolapse of the vagina can be caused by various reasons, which depend on the age, the presence of chronic diseases, the patient's lifestyle. It can be:
In girls, pathology is often associated with untimely trips to the toilet.
In old age, prolapse and prolapse of the vagina are associated with the loss of muscles and ligaments of elasticity, weakening of the muscles of the perineum.
Vaginal prolapse is very common immediately after childbirth, even in young patients or in women 40-50 years old who have undergone several births.
In the course of pregnancy, delivery, women develop functional insufficiency of the ligamentous apparatus, due to trauma during childbirth, the pelvic muscles suffer, tears appear in the perineum, which are often incorrectly stitched, become infected. All of these factors contribute to the prolapse of the vagina.
The development of muscle weakness is facilitated by the passage of a large fetus through the birth canal. If the method of delivery is chosen incorrectly (an episiotomy should be performed), the woman runs the risk of getting the walls or the entire vagina prolapsed at the birth of a child.
Too short a period of postpartum rehabilitation is also a risk factor for women with weak muscles and ligaments of the pelvic organs.
In addition, untreated partial or complete vaginal prolapse can interfere with the onset and healthy course of pregnancy, provoke miscarriages, premature birth.
Treatment of pathology is carried out taking into account the type, degree of organ prolapse, the patient's age, and the presence of concomitant diseases.
Treatment of the first stage of the disease begins with the appointment of a complex of physiotherapy exercises - Kegel gymnastics. The exercises are designed to strengthen the muscles of the perineum and make the ligaments more elastic. You need to do it regularly anywhere, several approaches a day.
Stage 1 consists of exercises to slowly squeeze the intimate muscles, followed by relaxation (tighten the vaginal muscles, as if you want to stop the process of urination). Start by squeezing for a count of 3 and work up to 20 seconds or more. Having mastered this exercise, proceed to the second stage.
2nd stage - dynamic contractions. Tense and relax the vaginal muscles very quickly. Start with 10 exercises, 5 sets per day, double the number after a week, gradually bringing the number of quick contractions and relaxations to 100-150 per day. Only having mastered the first two stages, you can proceed to the third.
3rd stage - pushing out. Tighten, as in constipation, childbirth and stay in this state for a few seconds. Gradually increase the time of tension of the intimate muscles. When performing the exercise, you should feel the tension of the muscles of the peritoneum and perineum.
In addition to practicing at home, it is useful to attend gynecological massage sessions, do Kegel exercises on simulators.
 In addition to physical therapy, you can return the vagina to its normal anatomical position with the help of special implants: plastic uterine rings (pessaries), which are placed in the vagina to prevent prolapse. They will hold the uterus in the correct position. Such treatment is an alternative to surgery when surgery is contraindicated. It is used for slight omission, in old age.
In addition to physical therapy, you can return the vagina to its normal anatomical position with the help of special implants: plastic uterine rings (pessaries), which are placed in the vagina to prevent prolapse. They will hold the uterus in the correct position. Such treatment is an alternative to surgery when surgery is contraindicated. It is used for slight omission, in old age.
Surgical treatment for vaginal prolapse is one of the most effective. With the 2nd and 3rd degree of vaginal prolapse, colporrhaphy is prescribed, colpoperineorrhaphy to raise the organs inside the pelvis. The operation is performed under general anesthesia and consists in removing part of the vaginal mucosa, suturing the stretched muscles, and the vaginal membrane. If the uterus has fallen out, then it is fixed with ligaments. A bandage should be worn after the operation.
Recipe number 1: baths
Treatment of incomplete vaginal prolapse can be supplemented by taking a sitz 10-minute soak with dope. To prepare an infusion of 20 g of herbs, pour 7 liters of boiling water and hold it in a water bath for 15 m. Cool the broth to 38 ° C before use.
Recipe number 3: alcohol tincture
Alcohol tincture with astragalus root in a ratio of 1/9 is also very effective in fighting vaginal prolapse. Insist the roots in a cool, dark place for 14 days. Drink 1 tsp of the strained tincture. three times a day before meals for a month. Do not forget to drink the tincture with plenty of water.
The prolapse of the vagina during pregnancy, after childbirth, in any other period of life can be prevented by following a number of recommendations and a simple set of exercises.
Prevention includes a special complex of exercise therapy during pregnancy, after childbirth, limitation of heavy loads, control over the development of multiple pregnancies, a large child.
Prevention is important after a difficult birth and beyond. Do regularly such simple exercises as "bicycle", "scissors", raise your legs with a roller under the buttocks and without, try to do "swallow", it is also useful to stand on one leg and do circular rotations with the other leg (you can lean on something) ...
It is important to try to pull the vulva up when walking. When urinating, try to squeeze the stream several times.
Also shown is a diet with a lot of plant fibers (vegetables, fruits).
If you have had an operation, when performing any physical work, wear a bandage to support the internal organs.
ekoaist.ru
There are a lot of factors that can contribute to the onset of this pathology, and these include:
Experts divide vaginal prolapse into three degrees, which differ in the severity of the pathology:
In addition, vaginal prolapse can be caused by the displacement of specific pelvic organs. So, share:
The prolapse of the walls of the vagina does not occur by itself - it is a symptom of a general change in the location of other internal organs in this area - they create pressure on the walls of the vagina.
Some of the symptoms of this pathology are felt by the woman herself, but the exact diagnosis is made by a specialist doctor during a detailed examination.
 Often this is accompanied by uterine hypertrophy, polyps of the cervical canal, pseudo-erosion. As a result of what is happening, dryness of the vaginal mucosa, its thickening or thinning, is manifested.
Often this is accompanied by uterine hypertrophy, polyps of the cervical canal, pseudo-erosion. As a result of what is happening, dryness of the vaginal mucosa, its thickening or thinning, is manifested.
In the study, it often turns out that microcirculation is impaired due to sclerotic changes in the lymphatic and blood vessels.
Already in the first stages of the disease, women feel painful impulses in the lower back, lower abdomen, experience difficulty with active movements, and her ability to work is noticeably reduced.
There is tissue irritation, itching, severe dryness of the mucous membrane. This often leads to the appearance of erosions (ulcers) in the vaginal area. Sex with vaginal prolapse is painful.
The prolapse of organs provokes frequent urination, urinary incontinence, sometimes the opposite reaction occurs - urinary retention.
Almost always, vaginal prolapse is accompanied by intestinal dysfunction - constipation occurs, uncontrolled gas separation, hemorrhoids appear, and cases of fecal incontinence are noted.
In the treatment of prolapse of the vaginal walls, both surgical and conservative methods can be used.
 These include the establishment of a pessary. Made of silicone or plastic, this internal organ support device is inserted into the vagina. Such a procedure is rarely resorted to, only when urgently needed.
These include the establishment of a pessary. Made of silicone or plastic, this internal organ support device is inserted into the vagina. Such a procedure is rarely resorted to, only when urgently needed.
The device is selected individually for each patient. Women who have it installed are under the constant supervision of a specialist, since complications are possible:
To prevent these phenomena, the doctor prescribes douching, rinsing, it is possible to change the model of the device.
Such treatment is allowed only with moderate prolapse of the vaginal walls. If it is not possible due to weakness of the vaginal muscles, a hysterophore is used. This device helps to hold the uterus with a pessary tied to a band that is attached to the waist.
Such methods are a typical palliative, which almost never leads to a complete recovery. Therefore, most often the most effective is surgical intervention, unless it is clearly contraindicated.
The technique of surgical intervention is chosen by a specialist depending on the degree of development of the pathology, the patient's age and the individual characteristics of her body.
Gymnastic exercises give a good effect in lowering the vagina. Performing them, you must definitely monitor your breathing.
The exercises are performed while lying on their backs or standing on all fours.

There is a well-known set of Kegel exercises that allows you to strengthen the muscle walls of the pelvic region. They are simple and accessible to every woman at any time of the day:
It is therapeutic gymnastics that becomes the main tool that helps to completely get rid of such a pathology without resorting to surgical intervention.
ladyinform.com
Treatment of prolapse of the vaginal walls.
The prolapse of the vaginal walls, subject to early diagnosis, can be eliminated conservatively; in more advanced and complicated cases, surgical intervention is performed. Timely treatment significantly reduces the risk of complications.
Conservative therapy.
Therapy is indicated for insignificant prolapse of the vaginal walls and is expressed in the use of a set of exercises, the purpose of which is to increase the muscle tone of the pelvic floor, including Kegel exercises (compression and relaxation of the muscles of the perineum), physical therapy. At the same time, therapy is prescribed for the general strengthening of the body, while nutrition is not of the last importance (no heavy foods that can cause constipation and complicate the problem).
During menopause, women are shown hormone replacement therapy in order to improve blood circulation and strengthen the muscles and ligaments of the pelvic organs.
If an operation is contraindicated for a woman for any reason, to prevent complete prolapse of the uterus, the patient is fitted with uterine rings (pessaries) - a device to support the internal organs is inserted into the vulva. The pessary is selected for each patient individually, after which regular observation by the gynecologist is shown, in order to exclude the development of serious complications (processes of a purulent and ulcerative nature, irritation and swelling of the mucous membrane, ingrowth of the pessary into the cervix or vulva). To prevent these phenomena, the doctor prescribes douching and washing the vagina. If the weakness of the vaginal muscles does not allow the introduction of the pessary, then a hysterophore is used - a device that holds the uterus through a pessary connected to a bandage attached to the waist.
Gymnastics (a set of exercises) with the lowering of the walls of the vagina at an early stage (can be used as a prophylaxis of the disease).
Exercises on all fours:
Exercises lying on your back.
Exercise should be done slowly and with control of your breathing. Do it two hours before meals or two hours later. The time for classes is not limited.
Kegel exercises.
Surgery for prolapse and prolapse of the vaginal walls (plastic of the vaginal walls).
After examining the patient with the participation of a proctologist and urologist, the doctor prescribes treatment, taking into account the severity of the pathology, the degree of loss, the patient's age and the individual characteristics of her body. As a rule, surgical treatment with plastic elements is recommended. This is mainly colpoplasty, which involves suturing the vaginal walls. There are two types of colpoplasty:
Surgical intervention is carried out using general anesthesia. The choice of the procedure for the operation is determined by the surgeon, taking into account the visual and video colposcopic examination, the analysis of the condition of the tissues of the walls of the vulva and the presence of concomitant diseases of the pelvic organs.
Postoperative period.
After assessing the general condition of the patient after the intervention, the doctor discharges her, usually on the second day after the intervention. To prevent the development of complications and accelerate the recovery period, it is necessary to strictly follow all the doctor's recommendations, namely:
Modern equipment and microsurgery capabilities make it possible to carry out an operation with low trauma. After the intervention, there are no visible traces and scars on the body.
Prevention of prolapse of the vaginal walls.
Treatment of prolapse of the vaginal walls with folk remedies.
Treatment with traditional medicine can only have an effect at an early stage and in combination with other therapies prescribed by a doctor, including exercise.
Quince can be brewed and drunk in the form of tea, it gives tone to the muscles of the uterus. For 100 g of dried fruits and a liter of water, brew in a water bath.
Alcohol tincture of astragalus root is also considered an effective traditional medicine against this ailment. For a part of the chopped roots, take nine parts of vodka. Keep the mixture in a cool, dark place for two weeks. Then strain. Take three times before the main meal (breakfast, lunch, dinner) with plenty of water. The treatment course includes thirty days, if necessary, the course can be repeated after two weeks.
Mix 50 g of lime blossom and lemon balm each, add 70 g of white ash and 10 g of alder root. Grind the mixture. Take two tablespoons, boil 200 ml of boiling water and insist until it cools completely. Take half a glass three times daily before meals. The course of treatment is twenty-one days, after two weeks of a break, the course can be repeated.
Datura is effective as a sitz bath for partial drooping. Pour 20 g of grass with seven liters of boiling water and keep in a water bath for fifteen minutes. After that, the infusion should be cooled to 38 degrees. Use for a sitz bath, which lasts no more than ten minutes.
prosto-mariya.ru
The prolapse of the walls of the vagina is a pathology that is associated with a decrease in muscle tone in the small pelvis, a weakening of the ligaments that support the natural position of the organs. Under the influence of certain factors, the uterus begins to descend, pressing on the vagina, which leads to its displacement. In the most severe cases, the pathology ends with the prolapse of the walls of the vagina outward.
According to statistics, this is a very common problem. Every third patient over 45 years old suffers from vaginal prolapse of one degree or another. Despite the fact that older women are more susceptible to the disease, it is also diagnosed in young women, however, their weakening of ligaments and muscles is associated with complicated childbirth. It is believed that each subsequent birth increases the likelihood of a similar problem in the future by several times. In nulliparous patients, prolapse of the uterus and vaginal walls is also possible, but it is usually associated with congenital abnormalities of the connective tissue.
The prolapse of the vaginal walls is not an independent disease - it is only a consequence of other problems. Currently, there are several risk factors:
During the diagnosis, it is very important to establish what exactly triggered the displacement of the genitals, since therapy largely depends on this.
The prolapse of the vagina progresses gradually, therefore, at the initial stages, signs may not appear at all. Occasionally, women are worried about pulling pains in the lower abdomen, which, however, are ignored, because they are perceived by the patient as symptoms of premenstrual syndrome.
As the organs are displaced, normal blood circulation is disrupted. This leads to thinning and excessive dryness of the vaginal mucosa. Some women notice a decrease in sensitivity during intercourse. Sometimes sexual intercourse is accompanied by severe pain.
Subsequently, small erosions appear on the vaginal mucosa. The list of symptoms also includes uncharacteristic vaginal discharge, sometimes mixed with blood. Some women complain of a constant foreign body sensation in the vagina, which is associated with displacement of the uterus and intestines.
The features of the course of the disease also matter. For example, the prolapse of the anterior vaginal wall affects the function of the bladder. Frequent urination is observed. Many patients complain of incontinence, periodic urinary leakage. Another picture is also possible - there is stagnation of urine in the bladder, which leads to the development of chronic forms of inflammation (cystitis).
The prolapse of the posterior wall of the vagina is associated with disruption of the intestines. Women with a similar diagnosis suffer from constant constipation, uncontrolled gas emission. Pathology increases the risk of hemorrhoids or exacerbation of existing hemorrhoids. In the most severe cases, fecal incontinence develops.
It is worth noting that the symptoms of vaginal prolapse directly depend on the stage of development of the disease. There are three stages in the progression of the disease.
The weakness of the ligamentous apparatus can be expressed in different ways.
As a rule, a simple gynecological examination is sufficient to suspect the presence of a prolapse in the patient. Of course, in the future, additional examinations are carried out:
Such treatment is possible only at the initial stage of the development of pathology. In this case, it is very important to strengthen the muscles of the pelvis, vagina, and abdominal wall. All this helps to distribute the load and relieve tension from the pelvic ligaments. Also, patients are recommended courses of therapeutic massage, which also improve blood flow to the pelvic muscles, provide the tissues with normal nutrition, strengthen the ligaments, and prevent congestion.
Some patients get a pessary, a special device made of special plastic or silicone that is inserted into the vagina and supports the cervix. It should be noted right away that this is a temporary measure. Installing a pessary only prevents the organs from dropping. Moreover, wearing such a device carries some risks. The list of possible side effects is as follows:
That is why doctors recommend that patients periodically change the models of this device. In addition, douching should be done daily to help avoid inflammation and suppuration. Pessaries are installed only if the operation when the vagina is pushed down is impossible for one reason or another.
Special exercises for lowering the vagina really help to strengthen the muscles and ligaments, activate blood circulation. This is unlikely to help return the displaced organs to their natural position, but it will definitely prevent their further prolapse. A set of Kegel exercises must be done every day:
There are other exercises that will also have a positive effect on the functioning of the organs of the reproductive system:
Today, only surgery is a truly effective method of therapy. The choice of the procedure depends on many factors, including the patient's age, her intentions to have children, the presence of accompanying complications, as well as the form and stage of such a pathology as vaginal prolapse. The operation can be performed in different ways:
This is how the prolapse of the vagina is eliminated. The operation is performed under general anesthesia. Within two days after the procedure, the patient should be under the supervision of a doctor. During rehabilitation, it is important to adhere to some rules:
If the patient had a prolapse and she completed the full course of treatment, then pregnancy is possible. After the transferred pathology in a mild form, which was eliminated with the help of exercises and other methods of conservative therapy, childbirth can take place naturally. If the treatment of prolapse was carried out surgically, then you cannot do without a cesarean section.
There are some folk recipes that help improve blood circulation in the pelvic organs, prevent the development of the inflammatory process and the appearance of erosion.
Of course, such medications can only be used as adjuvants - they help the body recover faster after therapy. In any case, before using the decoctions, you should definitely consult your doctor.
You already know why vaginal prolapse develops in most cases. Photos, symptoms, treatment methods are, of course, important questions. But if you adhere to some rules, then you can significantly reduce the risk of such a problem:
It is important to see your doctor as soon as you notice the first alarming symptoms of vaginal prolapse. Experts' reviews indicate that the disease is much easier to treat if the therapeutic measures were started in the early stages of the development of pathology.
fb.ru
The prolapse of the posterior wall of the vagina is one of the most common pathologies of the female reproductive system. This diagnosis is made by almost every second representative of the fairer sex, who has crossed the fifty-year mark. But in recent years, the prolapse of the posterior wall of the vagina has been observed in younger women - from 30 to 45 years old. 
Uterine prolapse: causes
The main cause of this pathology is age-related stretching of the ligaments of the uterus, but, as a rule, the prerequisites for this are created even in youth. The prolapse of the vaginal walls is facilitated by:
Symptoms of the disease 
Descent of the posterior wall of the vagina is accompanied by the following symptoms:
What does this disease lead to?
In the main number of cases with such a disease, changes occur in the location of many organs of a woman, and not only the genitals. The rectum and bladder suffer from this pathology. If you do not take all the necessary measures on time, then with the further process of prolapse, a hernia of the vaginal walls may form, as a result of which the bottom of the bladder, the walls of the rectum and intestines may go down. As a result, the patient begins to complain of constant urge to urinate and even urinary incontinence.
Prolapse of the uterus: surgery 
Treatment of this pathology is reduced to surgical intervention. In rare cases, they resort to orthopedic getting rid of this ailment using a pessary. The surgical solution to this problem lies in the process of suturing the vaginal walls. These procedures are performed by means of colpoplasty, which is divided into two types:
Which type of operation will be used in a particular case depends largely on the condition of the tissues of the vaginal walls themselves and on the presence of diseases of the pelvic floor organs. Colpoplasty is performed under spinal or general anesthesia. Here, the choice is made by the patient herself or the doctor, who, after a visual examination or calposcopic examinations, must determine the approximate time for the operation.
www.syl.ru
When the vagina is pushed down, one of its walls hangs down into the lumen of the vagina. Due to the fact that the bladder is located in front of the vagina, when its anterior wall hangs down, the bladder also begins to descend. This condition is called cystocele. The rectum is located behind the vagina, therefore, when the posterior wall of the vagina descends, the rectal wall, or rectocele, is also observed.

When the uterus descends, its downward displacement is observed, and with pronounced prolapse, the uterus may even "fall out" of the vagina. Of course, when we talk about "prolapse", we do not mean that at one point the uterus will break away from the body and fall to the floor. In spite of everything, the uterus remains securely attached to the body, however, when the uterus prolapses, it begins to "peek" out of the vagina.
Normally, the pelvic organs (ovaries, fallopian tubes, uterus, vagina, bladder, and rectum) are kept suspended by the muscles and ligaments of the pelvis, which in turn attach to the skeleton. The design is rather complicated, and a separate lecture on anatomy can be devoted to the structure of the pelvic floor (the structure that holds all the listed organs in place). But we will not go into details, it is enough just to understand that the vagina and uterus occupy the place assigned to them by nature, not just like that, but thanks to the muscles and ligaments of the small pelvis.
With age, the tone of the pelvic floor muscles decreases significantly, and the ligaments can stretch, therefore, with menopause, prolapse of the vagina or uterus is often observed. Among other things, the decrease in the level of estrogen in the blood, observed with menopause, also promotes relaxation and stretching of the ligaments.
An increased risk of prolapse of the genitals during menopause is observed if:
It happens, and even more: in most cases, in the early stages of prolapse of the vagina and uterus, there are no symptoms. There is no need to doubt the correctness of the diagnosis if the gynecologist discovered a prolapse, and you do not have signs of this disease.
With cystocele (prolapse of the bladder wall), symptoms such as frequent urination, urinary incontinence, involuntary urination, and urinary retention may appear. Learn more about menopause urinary incontinence.
With rectocele (prolapse of the rectal wall), difficulties arise during bowel movements, when more effort is needed to empty the intestines than before.
1 degree of prolapse of the uterus: the cervix is not above the vagina, as it should be normal, but descends into the vagina.
2 degree of prolapse of the uterus: the cervix descends to the entrance to the vagina.
3 degree of prolapse of the uterus: the cervix "looks out" from the vagina.
4 degree of prolapse of the uterus: the entire uterus "peeps" out of the vagina. This condition is also called prolapse of the uterus.

The diagnosis of prolapse of the genitals can be made during an examination by a gynecologist. Your doctor will examine you while lying down and standing. Due to the fact that with an increase in intra-abdominal pressure, the prolapse of the vagina or uterus becomes more noticeable, the doctor will ask you to cough or push.
The gynecologist may also prescribe the following tests:
A prolapse of the vagina or uterus does not always need to be treated. If you do not feel any symptoms, nothing bothers you, and the gynecologist found a slight or moderate prolapse, then no treatment is prescribed. Your gynecologist will recommend several exercises that strengthen your pelvic floor muscles and ligaments, and will recommend that you come back for a follow-up check in 6-12 months.
If you have symptoms of prolapse, then you will need treatment: some can be done at home on your own, and some can be done by your doctor.
If you have a prolapse of the walls of the vagina or uterus, heed the following advice from gynecologists:
When the vagina or uterus prolapse, conservative treatment (pessaries and hormone replacement therapy) or surgery may be prescribed.
Your gynecologist may recommend that you wear a special device that supports the uterus and prevents it from dropping below a certain level. Such devices are called “pessaries,” or simply uterine rings (although there are other forms of pessaries, not just rings).
 If the gynecologist thinks that you can independently remove and install the pessary, then he will teach you how to do it correctly. In some cases, the pessary has to be worn all the time, in other cases it will need to be removed before bed. With a slight prolapse of the vagina or uterus, the pessary will need to be installed only before long walks, physical activity, etc.
If the gynecologist thinks that you can independently remove and install the pessary, then he will teach you how to do it correctly. In some cases, the pessary has to be worn all the time, in other cases it will need to be removed before bed. With a slight prolapse of the vagina or uterus, the pessary will need to be installed only before long walks, physical activity, etc.
The pessary does not cure prolapse of the uterus, but it helps to eliminate the symptoms of this condition and make your life much easier.
The leading cause of prolapse of the vagina or uterus during menopause is the lack of estrogen hormones in the blood. Estrogen replacement therapy can be an effective method of strengthening the muscles and ligaments of the pelvis. Usually, with prolapse of the genitals, estrogens are used in the form of vaginal creams or suppositories, which must be injected directly into the vagina. On our site there is a separate article dedicated to this topic: Hormone replacement therapy for menopause.
If conservative treatment does not help, or there is a prolapse of the uterus of 3-4 degrees, then an operation is prescribed. The operation can be performed through an incision in the abdomen or through the vagina.
During the operation, the doctor can install a special implant - a structure that will hold the pelvic organs where they should be normal. In some cases, the gynecologist may recommend removing the uterus. There is a separate article on our website dedicated to the operation to remove the uterus.
After the operation, you will not be able to lift weights for at least 6 weeks, and for another 3 months you should avoid any situations in which prolapse of the genitals increases: constipation, coughing, smoking, weight gain.
www.mygynecologist.ru
The body of the uterus is displaced unevenly, the back or front surface descends downward. The process of lowering the posterior wall of the vagina, in which there is pressure on the rectum, is called rectocele. The early stage of this disease is almost asymptomatic.
The first thing that a woman begins to feel is pain during sex. For the disease in later stages, the following symptoms are characteristic:
At the last stage, a woman can no longer have sex. Simultaneously with the prolapse of the body of the uterus, erosion and other inflammatory processes occur.
The method of treating rectocele depends on the degree of prolapse; for this, ultrasound studies, urography, colposcopy are prescribed, laboratory tests are taken, smears and feces are examined.
Prolapse of the uterus is a serious disease, ignoring which always leads to irreversible consequences.
Early diagnosis will allow you to get rid of this problem at the first stage and avoid unpleasant consequences. What to do if a descent of the back wall is diagnosed with moisture, this disease is treated with an operative method, laser correction or conservative treatment.
Laser correction is a modern non-surgical method using modern technologies. This is the safest and most effective treatment for rejuvenating and restoring the turgor of the vaginal walls.
Surgical intervention is performed at 2 and 3 stages of displacement. During a surgical operation, surfaces are tightened and sutured, implants are implanted to fix organs. In addition to the above methods of treatment for vaginal prolapse, drug therapy is prescribed, as well as a gymnastic complex.
If the treatment of prolapse was not started on time, with advanced stages, the only way to eliminate organ prolapse is to use a surgical scalpel. Modern surgery offers women diagnosed with prolapse of the back wall moisture to perform an operation and at the same time plastic surgery. This type of colpoplasty is called posterior colporrhaphy.
The purpose of the operation is to remove excess tissue, narrow the vaginal opening, and restore the anatomical location of organs.
This surgery has its own characteristics. The surgeon needs to remove the extra tissue flap on the vaginal wall adjacent to the perineum. The size of the cut fabric should be such that the seams do not come apart after overstraining.
The first 3 - 4 days, patients are assigned to bed rest, the woman is under the supervision of a doctor in a hospital. The rehabilitation period after colporrhaphy lasts 1.5 months. At this time, you cannot:
Among the contraindications for colporrhaphy are venereal diseases, heart disease, acute stages of thrombophlebitis.
In milder forms of prolapse, the following help to restore the anatomical location of organs:
A woman who uses corrective rings must wear a bandage, observe the strictest hygiene and see a doctor.
A strict diet of plant fiber also helps. Foods with a high percentage of fiber help the easy passage of feces through the intestines. It is recommended to take laxatives and eubiotics that restore the intestinal microflora.
Along with diet, pharmaceuticals and physical therapy, it is recommended to use recipes from traditional medicine to help increase muscle tone. These are douching and baths with quince solution, decoctions inside from lemon balm, alder, linden color, white ash.
It is necessary to wear a supportive bandage for rectocele, especially for women after childbirth, when muscle tone is weakened. You cannot wear the device all the time, the body must get rest.
Physiotherapy exercises and special Kegel exercises will help restore the anatomical positions of organs and strengthen muscle tone. Exercise therapy is carried out at the first stage under the supervision of an instructor; in the future, a woman can perform a simple gymnastic complex on her own.
Exercises allow you to get the greatest therapeutic effect:
The Kegel complex is effective for genital prolapse. These are three simple but effective exercises: stepped tension and such relaxation of the pelvic muscles, delaying the stream during urination for a few seconds and moderate attempts, as in labor.
Specialists in aesthetic gynecology are successfully dealing with the problem of restoring the tone of the muscular structures of the vagina. Laser correction is performed using special medical equipment and takes up to 30 minutes. This non-invasive treatment is performed with a laser beam. With the help of a laser, excess tissue is heated and evaporated. Such technologies contribute to better regeneration, increased blood circulation, and the production of collagen fibers.
After the laser procedure, normal turgor is restored, the tissues acquire elasticity, and the volume of the vagina decreases. Discomfort disappears, the normal process of urination is restored.
The cost of laser therapy in aesthetic gynecology clinics depends on the degree of wall prolapse:
The prolapse of internal organs is a serious pathology, it is dangerous with unique consequences. The sooner the disease is diagnosed, the faster it can be cured.
netbolezni.net
The pelvic organs are fixed: with the help of ligaments, they are connected to each other, as well as to nearby structures. The fat capsule creates a kind of airbag for the bladder and kidneys, further immobilizing them. The muscles of the pelvic floor and the anterior abdominal wall keep the organs in an optimal position, preventing displacement. Due to the violation of several links, the uterus and vagina prolapse, which leads to disability.
In most cases, the disease occurs in women after 40-45 years of age, who have given birth several times. Pregnancy and childbirth tend to stretch the muscles of the pelvis, which increases the tendency to prolapse of the vagina. Less often, pathology occurs at a younger age, cases of uterine prolapse are described even in nulliparous girls.
The main reasons for vaginal prolapse include:
Symptoms of prolapse of the vaginal walls primarily depend on the severity of the process.
After a gynecological examination, the doctor determines the degree of the disease:
The disease in the initial stages develops gradually, but when the symptoms are well expressed, there is a sharp deterioration in the condition. Therefore, it is important to identify vaginal prolapse in the early stages in order to prevent complications.
The first symptoms are nonspecific and easy to miss. Women complain of discomfort during intercourse, intimacy is not enjoyable. These signs should be alarming, it is recommended to visit a doctor to find out the reason. The above manifestations are also observed in infectious diseases of the genitourinary system, psychological trauma, hormonal disorders.

Sex with vaginal prolapse becomes painful. A woman has a sensation of a foreign body in the vagina, with the progression of the disease, a protrusion from the genital slit appears.
The clinical picture depends on the degree of damage to nearby organs. The prolapse of the anterior wall of the vagina is accompanied by impaired urination. Disturbed by frequent urge to use the toilet, urinary incontinence, soreness or itching in the area of the urethral opening. These changes are associated with a violation of the normal shape and location of the excretory organs. The bladder, along with the ureters, is located in front of the vagina. With the weakening of the pelvic muscles, the wall of the bladder descends into the hernial protrusion, which leads to congestion, incomplete emptying, and the development of a bacterial infection. This phenomenon is called cystocele in medicine.
Descent of the posterior wall of the vagina occurs less frequently. In this case, the digestive system suffers. Problems with emptying come to the fore - constipation prevails. The bowel loop often falls into the hernial protrusion, thereby interfering with the normal movement of feces. Patients complain of bloating, discomfort. Pain during prolapse of the vagina can be localized in the lower abdomen or umbilical region. In rare cases, anal fissures, fecal incontinence, hemorrhoids occur.
The disease develops gradually. At the first stage, the protrusion does not go beyond the genital slit; it is almost impossible to see it visually. Stool and urination are not disturbed.
Discomfort during sex or lack of satisfaction with sex life goes unnoticed in most cases. Women associate this with fatigue and stress.
Thus, the symptoms of vaginal prolapse are mild or absent at the onset of the disease. Until the bladder or intestines are drawn into the pathological process, there will be no disturbances from the excretory system and digestive organs.
A gynecologist deals with the treatment of prolapse of the walls of the vagina or uterus. In severe cases, it is necessary to consult a proctologist, urologist, surgeon.
If there is a prolapse of the vagina or uterus, it is not difficult to make a diagnosis. In the early stages, when there are no visual changes, the doctor prescribes additional research methods. Often, symptoms resemble diseases of the urinary system or digestive organs. It is necessary to clearly distinguish between these conditions in order to choose the right treatment tactics.
Diagnostic measures include:

Pregnancy must be planned - a gynecologist's examination and tests are required. If the disease is detected in the early stages, this is not a contraindication to conceiving a child. Exercising when lowering the vagina can help strengthen your pelvic muscles. Regular exercise can help a woman get rid of her genital prolapse.
With the formation of a protrusion that goes beyond the boundaries of the genital slit, contains the bladder or intestines, surgical intervention is indicated. It is forbidden to get pregnant at this stage. After the operation, when the vaginal walls are pushed down, delivery is carried out by caesarean section. Physiological childbirth is contraindicated.
The choice of treatment tactics depends on many factors. The doctor takes into account the woman's age, the degree of loss, the presence of complications, concomitant diseases, the need to preserve fertility. There are several methods for treating vaginal prolapse: surgery, conservative therapy, the use of traditional medicine, special exercises, exercise equipment, and gymnastics. The most effective is an integrated approach - a combination of several methods.
If the disease was detected in the early stages, surgery can be avoided. The doctor prescribes exercises to strengthen the pelvic floor, abdominal muscles.
With a weakened tone of the vaginal muscles, the use of a special ring is shown, which keeps the cervix in a normal position. The pessary for lowering the vagina is selected individually, depending on the severity of the symptoms. The ring is inserted towards the cervix in an oblique position, then it is aligned, resting against the pelvic floor and the pubic joint on the other side. In this way, the vagina is fixed, which prevents prolapse.
Patients with a pessary in place should be monitored regularly by a doctor. Improper use, neglect of the rules for caring for the ring during vaginal prolapse leads to complications.
Possible consequences:

To avoid complications, the doctor prescribes regular douching, rinsing the pessary. From time to time it is necessary to change the model, the shape of the ring, use tampons.
Special devices are used to strengthen the muscles of the pelvic floor and abdominal wall. The bandage for lowering the vagina is a high panties made of elastic material, which are worn under clothing. This allows you to stabilize intra-abdominal pressure and muscle tone.
This method is effective for lowering the vagina after removing the uterus, second or third births, and inserting a pessary. Also, the bandage is used for prophylactic purposes, in the presence of risk factors.
Exercise is the best way to strengthen your pelvic and perineal muscles in the early stages of the disease. The main condition is regularity. Gymnastics for lowering the vagina includes exercises for the abdominal press, back.
The following exercises are most effective:
In addition to general strengthening gymnastics, Kegel exercises are effective when lowering the vagina. The complex is specially designed to increase the tone of the intimate muscles. A big plus is that the exercises can be performed anywhere: at work, in transport, at home. They are completely invisible to strangers. It is recommended to repeat the complex up to 5-6 times a day, gradually increasing the number of approaches. For greater effect when lowering the vagina, exercise machines are used.
Execution rules:

When the vaginal wall is lowered after childbirth or the removal of the uterus, when the protrusion goes beyond the genital slit, the operative restoration of the normal location is shown. The surgeon takes into account the severity, the presence of concomitant diseases, the involvement of nearby organs in the process. If there are no contraindications (diabetes mellitus, severe heart disease, lung disease, kidney failure), the doctor chooses the most appropriate method of plastic surgery.
When the anterior wall is lowered, colporrhaphy (suturing) of excess vaginal folds is shown with the restoration of the physiological arrangement of organs. During colpoperineorrhaphy, the surgeon sutures the posterior wall of the vagina to the muscles of the perineum, strengthening the septum.
After surgery, antibiotics, anti-inflammatory suppositories, ointments, antiseptics are prescribed for quick wound healing.
To prevent recurrent vaginal prolapse after surgery, several rules must be followed.:
Decoctions, teas, infusions can complement treatment in the early stages - traditional medicine alone is not enough. All appointments must be made by a doctor. It is not recommended to use recipes on your own, since some herbs negatively affect the genitourinary system, cause bleeding.
The following decoction increases the tone of the uterus. It is necessary to take in equal proportions linden and lemon balm flowers (50 grams each), add a tablespoon of alder root and 80 grams of white ashberry. Mix the ingredients, steam with boiling water. Consume 100 ml of broth before meals for 3 weeks.
To prevent the development of the disease, if there are risk factors, you must follow simple rules:
A decrease in the tone of the pelvic floor muscles is not only a cosmetic problem, it is a serious disease of the genitourinary system. If you experience discomfort, pain during sex, or violations of urine flow, it is recommended to consult a gynecologist. Early diagnosis will help prevent the development of the consequences of vaginal prolapse, avoid surgical treatment.
Vaginal prolapse is positioned as a pathological condition of the female genital organs. The main cause of this disease is the weakness of the pelvic floor muscles.
Recently, this disease has rejuvenated. So, ten out of a hundred patients with such problems are not even thirty years old. About twenty percent of all cases are women aged 30 to 45 years. Moreover, not in every case the reason lies in the fact that a woman has recently given birth to a child. So, there are isolated cases when the disease affected young girls and even virgins.
Looks like a visual and physiological change in the normal placement of internal intimate organs. At the same time, the muscles of the abdominal region and the pelvic floor are weakened. This is because too much pressure was recorded inside the abdominal region, which led to a deterioration in the elasticity of the ligaments. It turns out that they can no longer keep internal organs in their normal placement. This means that the woman loses muscle tone, and the tissues of the vagina begin to sink down.
The disease is characterized by a rather slow rate of development at the very beginning and active progression, provided that it is not treated in time. Plus, it can lead to inflammation.
The disease affects either the anterior or posterior wall of the vagina. However, it also happens that both walls go down at once. Practice shows that it is the lowering of the front wall that is the most frequent. At the same time, in addition to everything, the woman's bladder with the urethra also begins to descend. If the back wall of the vagina falls, parallel prolapse or even prolapse of the rectum begins. For this reason, the patient should be ready for a full examination by several specialists of different profiles at once, because this is the only way to achieve complete recovery.
In the early stages, this disease does not manifest itself at all. The only thing a woman can pay attention to is painful sensations during intercourse. In addition, some heaviness and a feeling of increased pressure in the vulva may begin, after which inflammation, swelling of the vaginal opening, and unpleasant urination begins. Incontinence of urine, gas and feces can also be recorded. In the abdomen, pulling pains begin, the lumbar region experiences increased stress.
The prolapse of the anterior vaginal wall is often accompanied by chronic cystitis due to urinary stagnation. The back wall brings the feeling of a foreign object (fullness) to the vulva.
Only a gynecologist can detect a disease in the early stages during an examination on a gynecological chair. The doctor can easily notice the walls protruding from the vagina. First, the gynecologist carefully adjusts them, and then assesses the condition of the pelvic floor muscles. After that, the patient is referred for additional examinations to determine if there are additional problems.

- this is not a sentence for women who want to feel the joy of motherhood. There are many examples when both young and older women, after such cases, could still give birth to a child. However, it is necessary to focus on the stage of development of the disease. So, if the disease is in the first stage, it is possible to become pregnant and give birth to children, even without prior surgery. If the disease is at the second or more stage, an appropriate operation must be performed. Only under this condition can a woman become a mother. Otherwise, the risk of prolapse of the uterus cannot be avoided.
It is also important that after an operation to restore the muscles of the vagina, a woman will not be able to give birth on her own: the child will be born exclusively by cesarean section.
Such a disease, depending on the stage, can be treated both conservatively and promptly. The risk of complications with any of these approaches will be minimal.
Conservative therapy consists of specific exercises that work to develop and strengthen the pelvic floor muscles. In addition, the doctor prescribes a specific diet, which must be strictly followed.
The operation is prescribed in difficult stages that conservative therapy cannot cope with. It is carried out mainly under general anesthesia, but local anesthesia is also possible at the second stage. Recovery after surgery takes several days.
Sign up for a consultation with a gynecologist by phone
or on the website of the Clinic of Innovative Technologies

Prolapse of the vaginal walls (vaginal prolapse) is a pathology that most often occurs after delivery or in women with menopause. The disease is characterized by the appearance of discomfort and pain in the vagina.
Vaginal prolapse is a disease that may not manifest itself for a long time. The mechanism for lowering the vaginal walls is as follows:

The muscular walls of the vagina perform vital functions. They provide not only the natural immobility of the pelvic organs, but are also responsible for achieving orgasm (due to active contraction). Therefore, it is very important for a woman to immediately consult a specialist when the first signs of vaginal prolapse are detected.
The prolapse of the walls occurs due to the increased pressure of internal organs, which occurs against the background of atrophy of the pelvic floor muscles. Very often, prolapse of the anterior or posterior wall of the vagina is diagnosed in women who have given birth and in older women.

In addition, vaginal prolapse can occur in women who overload the body with excessive physical exertion.
Statistics indicate that in 3 out of 10 women, vaginal prolapse occurs as a result of frequent labor.
Additional causes of vaginal prolapse disease include:

As a result of the close connection between the vagina and the uterus, the process of prolapse occurs simultaneously. Therefore, the weakening of the ligamentous mechanism of the uterus is directly responsible for the weakening of the walls of the vagina.
Prolapse is an insidious disease that progresses slowly over 10-15 years. The exception is cases of obstructed labor, when the pathology manifests itself immediately after delivery.

Common symptoms experienced by patients include:
One of the clearest signs of prolapse of the walls is the sensation of a foreign object in the vaginal area.
In medicine, there are three degrees of vaginal prolapse.

Each degree differs in symptomatology and stage of pathological prolapse.
| Pathology degree | Characteristic | Symptoms |
| First degree | The cervical pharynx is practically not lowered and is located at a distance of 20-30 mm. from the entrance to the vagina. There is also a slight expansion of the genital gap, however, under the influence of efforts, the gap can be closed. |
|
| Second degree | There is a significant prolapse of the cervix, which is found at an appointment with a gynecologist. The doctor notes a pathological displacement of the pharynx to the vestibule of the vagina. Also, a specialist may notice that with significant attempts, the pharynx moves outward, but after that it is set back. |
|
| Third degree | As a result of the weakening of the walls of the vagina, their ability to hold the cervix decreases, which leads to prolapse of the uterus and contact of her body with underwear. This leads to cracks in the mucous membrane and to the colonization of pathogenic microorganisms. These unpleasant processes lead to progressive inflammation of the cervical canal. |
|
Some sources indicate four stages of pathology. The final stage means complete prolapse of the walls and uterus.
In addition to the highlighted three degrees of vaginal prolapse, in gynecological practice, two types of this ailment are distinguished. The first type is called cystocele - a pathological process of prolapse or prolapse of only the anterior wall of the vagina, accompanied by a change in the position of the bladder, which provokes prolapse of the vaginal wall.

The second type is rectocele (prolapse of the posterior wall of the vagina). This type of pathology is accompanied by the appearance of the so-called "pocket" in the rectum, which contributes to the accumulation of feces and the formation of chronic constipation.

To identify pathology, the doctor examines the patient in the gynecological chair. The specialist pays special attention to the anatomical location and external state of the vaginal wall (anterior and posterior), urethra, cervix.
The main actions of the doctor during the examination are as follows:

In addition to the examination, the gynecologist directs the patient to the urologist for a procedure such as a urodynamic study (they check the function of emptying the bladder, a violation of which indicates a problem). Also, an ultrasound scan, which shows what the uterus and ovaries look like, are considered mandatory diagnostic methods.

The earlier the prolapse of the vaginal walls is diagnosed, the higher the likelihood of a favorable outcome from conservative treatment. Otherwise, the patient is prescribed surgery.
The term "conservative treatment of the lowering of the walls of moisture" means therapy using a set of exercises that are aimed at increasing the tone of muscle tissue. Therapeutic exercises include the following exercises:


If the effect of therapeutic exercises is not observed, and surgery is contraindicated for any reason, the specialist installs the uterine ring inserted into the vulva (pessary). This ring helps to keep the internal organs from falling out.
After the introduction of the uterine ring, the patient should systematically observe the attending physician, since the pessary can grow into the mucous membranes, causing such pathological phenomena as suppuration, inflammation of the mucous membrane and irritation.

In addition to physical therapy, the doctor prescribes the intake of fortifying medications, which include vitamin complexes (Selmevit, Complivit, Triovit) and wearing a bandage. Also, a separate place in the therapy of prolapse is given to proper nutrition, which is aimed at reducing the risk of constipation.
During menopause, a woman (in addition to exercise therapy) is prescribed a course of hormone therapy, which is aimed at normalizing the patient's hormonal levels, improving blood circulation, and restoring the elasticity of the vaginal muscles.
When diagnosing a prolapse of the walls of the 3rd degree, a surgical operation is prescribed - colpoplasty (plastic, in which the walls of the vagina are sutured). Colpoplasty is of several types:


The type of operation is determined by a consultation of specialists. The decision is based on the degree of progression of the pathology, analysis of the epithelium of the walls of the vulva, the presence of concomitant pathologies or other health disorders of the patient.
0